You all think you know hospice. You don’t, and I will tell you why.
Hospice is a bastard child of the Medicare system. It went live in 1983 as a standalone entity during the Reagan administration and remains a disjointed program today. I would characterize its evolution as such: the road to hell is paved with good intentions.
Why is that?
When you go into hospice, your care path goes 180, and usual Medicare rules don’t apply. The benefit reroute sometimes makes life harder for families and patients. It’s like handing your keys off into the hospice kingdom–they run the show, and it’s both a blessing and a curse.
You are all familiar with the “likely to survive less than six months” limitation and how it impacts the treatment of the patient and the decision-making we are uncomfortable applying. We make someone hospice and everything changes. No more life-sustaining measures; no heroic technology; no cutting edge pharmaceuticals.
That also includes Medicare Advantage plans (a commercial plan overseeing the full spectrum of Medicare benefits. For newbies, here’s more). You go hospice, and you get disenrolled* from MA and funneled into the hospice path. If you think MA should be responsible for patients while in life (and death), it makes no sense to separate the two. MA combines Mcare parts A, B, and D, so why not hospice? But it is what it is.
Payment is different for hospice, and it’s not customary Medicare fee for service. That explains the reluctance of many hospices to take on the costs of many of the things we might like them to do. That’s the lesson and the reason for the failing grade: providers do not know this. Hospices get one per diem rate for care and given what patients require expenses often do not meet needs.
There are four levels of care (and payment), and we distinguish them by labor and intensity:
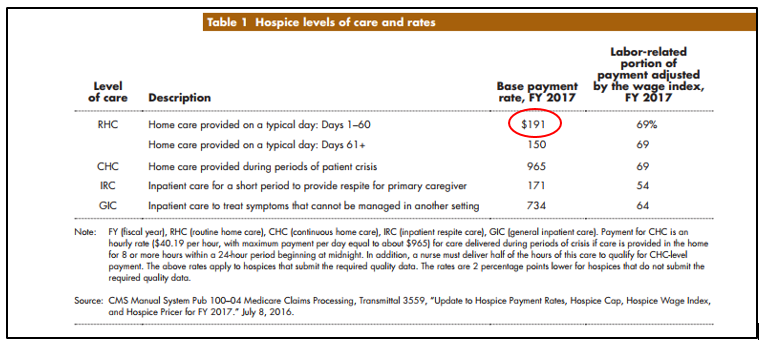
95% of hospice service is RHC (routine home care), and it reimburses $191 per day. You can see the other levels and their respective payments. That’s all the hospice provider gets—so if you want to give the patient an expensive antibiotic it comes out of the hospice’s program pool of funds. A problem. There are some CMS demonstrations going on now that test whether offering simultaneous hospice and treatment benefits improves QOL and outcomes, but answers will take time. We’ll see.
Anyway, this short briefer is excellent. Have a look, and it will help set you straight on the ins and outs of the benefit.
*Not quite “disenrolled” but a change in how an insurer, a Medicare Advantage provider in this case, defines a “covered” service.



Leave A Comment