Unless I have a pressing inpatient problem in need of a subspecialty consult, I defer to the outpatient setting. This goes double if the patient’s PMD practices elsewhere. You can guarantee any benefit of “urgent” consultation will be outweighed by the harms of siloed care and information drops when we set the patient adrift in the community. Better the patient sees a colleague of their regular doctor. At least the discharging doc will know treatment inertia moved in the right direction, lowering the risk of an adverse event.
Along those lines, we don’t have much outcomes data when providers disaggregate care. Folks move from a familiar to unknown clinical setting—and the EMRs of today can’t create order from chaos. Moreover, we know little when a patient, in the continuum of an episode of illness, leaves a hospital and then reappears in another facility days or weeks later. Until now.
Just released, Care Fragmentation in the Postdischarge Period: Surgical Readmissions, Distance of Travel, and Postoperative Mortality, looks at that very question. One of the authors, Ashish Jha, has appeared in the blog before, and publishes prodigiously on the subjects of quality and in particular, readmissions.
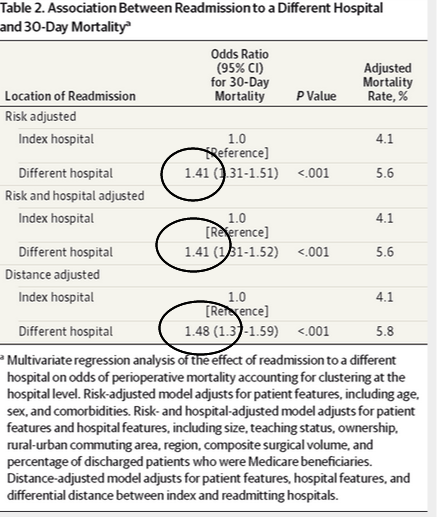
The authors looked at a large swath of readmitted surgical patients (93K)—all Medicare and undergoing major procedures–and focused on a subgroup presenting to a second hospital within 30 days of discharge (23K). They controlled for hospital-level covariates including size, teaching status, ownership, composite surgical volume, rural-urban status, distance from facility, and percentage of discharged patients who were Medicare beneficiaries.
What did they find?
Fragmented care, again, even after controlling for the usual suspects—especially distance, may contribute to a higher mortality rate. The absolute mortality difference was 1.7% (4.1% vs 5.8%), suggesting that if this effect were causal, one would have to avoid 59 readmissions to a different hospital to save one life.
With our experience in care transitions (not good), hospitalists should not find the data surprising.
Obviously, given the observational nature of the study, the use of administrative claims, and risk of confounding, the authors can only speculate disjointed treatment plays a part in outcome decline. However, it seems foolhardy to assign the results to chance alone.
The investigators conclude with policy solutions:
Although we are unsure why readmission to a different hospital is associated with higher mortality, our findings suggest an important area for hospitals and policy makers to focus their efforts. To improve outcomes for readmitted patients, hospitals might focus on 1 of 2 (or both) strategies. First, they could make more of an effort to bring patients with complications back to the original hospitals. Second, they might focus on improving continuity of care by focusing on better clinical data exchange and better clinical integration.
Obvious fixes and chants we have recited for years. It’s just a matter of when.
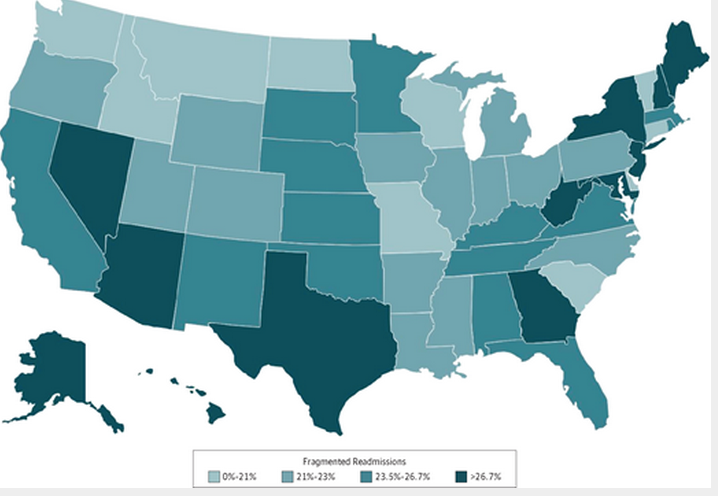
The paper also includes a map of fragmentation variation. No surprise, care is all over the map. No pun intended:


Leave A Comment