by Arjun Srinivasan, MD
I’ve had the privilege to work with many hospitalists over the past few years and I know that the problems caused by antibiotic overuse are ones that hit home for all of you. My guess is that you are rounding every day on patients who have infections caused by resistant bacteria and on patients who are suffering from C. difficile. Indeed, antibiotic resistance has become nothing short of a patient safety crisis as we are now encountering patients who have few, if any, antibiotic options available. This is obviously a life or death issue when we’re talking about patients who are immune compromised or critically ill with sepsis.
There is a lot of good data that shows that in hospitals, antibiotic stewardship programs can help reduce the complications of antibiotic overuse, like C. difficile and resistance, while also improving infection cure rates and saving money. It is for these reasons that CDC and SHM, along with many other private and federal organizations, have called for hospitals to implement antibiotic stewardship programs to improve antibiotic prescribing practices and reduce their inappropriate use.
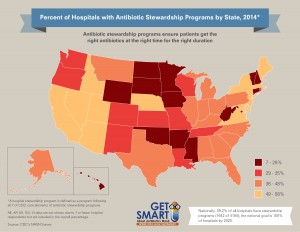 However, many hospitals have not implemented antibiotic stewardship programs. According to , only 39.2% of all U.S hospitals have antibiotic stewardship programs that meet all seven of CDC’s Core Elements for Hospital Antibiotic Stewardship Programs. There is clearly a lot of work to be done to reach the national goal of 100% of all U.S. hospitals implementing antibiotic stewardship programs by 2020. And I believe that hospitalists must play a central role in our efforts to improve antibiotic use in hospitals.
However, many hospitals have not implemented antibiotic stewardship programs. According to , only 39.2% of all U.S hospitals have antibiotic stewardship programs that meet all seven of CDC’s Core Elements for Hospital Antibiotic Stewardship Programs. There is clearly a lot of work to be done to reach the national goal of 100% of all U.S. hospitals implementing antibiotic stewardship programs by 2020. And I believe that hospitalists must play a central role in our efforts to improve antibiotic use in hospitals.
In many hospitals, it is hospitalists who likely have the greatest influence over how antibiotics are used since you are treating so many of the common infections that patients get admitted for. For example, in a survey done in 2011 in over 180 hospitals, the top three conditions for which antibiotics were given were community acquired pneumonia, urinary tract infections and skin and soft tissue infections. In fact, these 3 infections accounted for more than 50% of all hospital antibiotic use and are clearly “bread and butter” issues for hospitalists.
And beyond being important users of antibiotics, hospitalists are really skilled at leading quality improvement work. I’ve already seen firsthand how effective hospitalists can be in implementing stewardship interventions. I worked with the Institute for Healthcare Improvement on a pilot program of hospitalist-led stewardship efforts. What we learned from that experience is that one of the interventions that really resonated with hospitalists was the idea of taking an “Antibiotic Time Out”, which is a deliberate pause after about 48 hours of antibiotics to assess if the patient indeed needs an antibiotic, and, if so, what’s the best antibiotic and for how long? I’m also excited to be working with the University of Michigan and hospitalists around the state of Michigan on a new effort to focus on improving the treatment of some of the common infections that lead to antibiotic use. Finally, CDC is thrilled to be partnering with SHM on the Fight the Resistance Campaign.
I encourage hospitalists to improve antibiotic use and prescribing by:
- Looking at prescribing for common infections to see if there are opportunities to improve antibiotic use. CDC has developed some audit tools to help assess antibiotic use for some common infections that might be useful for quality improvement efforts.
- Taking leadership roles to improve their hospital’s antibiotic prescribing practices by using CDC’s Core Elements of Hospital Antibiotic Stewardship Programs as a resource to antibiotic stewardship implementation or expansion efforts.
- Encouraging their hospitals to participate in the National Healthcare Safety Network’s (NHSN) Antimicrobial Use (AU) Option to measure stewardship activities.
- The AU option provides a mechanism for facilities to report and analyze antimicrobial usage as a part of antibiotic stewardship efforts at their facilities.
- Printing and sharing educational fact sheets with colleagues at your facility.
- Joining SHM’s Fight the Resistance campaign to learn more about how hospitalists can improve antibiotic use.
Hospitalists’ commitment to antibiotic stewardship plays a critical role in protecting patients. It’s crucial that we improve appropriate antibiotic prescribing to ensure that the antibiotics we currently have work for patients when they need them the most. I thank you for your leadership as together we improve antibiotic use in our hospitals.



Leave A Comment