I left off last week’s post with a tease. If you recall, I made note of the frequent mentions med mal gets in the lay and professional press, as well as the outsized influence the threat of getting sued has on physician psyches.
Physician surveys, albeit with their biases, can tell us how we feel about medical torts. However, as a field, from those same surveys, we discern little of our actual risk.
Relative to our outpatient or subspecialty colleagues, the system has saddled us with a distinct data disadvantage. We have no unique identifier or tracking ability, so assessing suitable premiums and sussing out trends within our specialty–and where we fall short (or not), make corrective actions difficult.
It would be nice to have a study like this, for example, as the day may come when malpractice carriers disaggregate inpatient from outpatient claims. Our discipline has weaknesses for sure, like all fields, but we need to ascertain the risks unique to us—to better inform us in clinical and liability spheres.
Today, The Hospital Leader and the Journal of Hospital Medicine present online first access to a paper authored by Adam Schaffer, MD, and his group at Harvard. Their paper, Liability Impact of the Hospitalist Model of Care, gets to the heart of the questions raised above. Our release marks the first publication probing hospitalist liability risk in the peer-reviewed literature. My Q&A with Adam follows below (with brief edits for clarity):
Q: Adam, you have delved into a topic of great concern. Aside from payment and salary, medical malpractice garners outsized interest from physicians—particularly from a young field without a liability history. For those not familiar with your paper, tell us how you became interested in the subject and what you found?
Schaffer: I have had a longstanding interest in medical-legal issues, and medical malpractice is an issue that often arouses strong feelings and can be a source of significant anxiety for physicians. As you said, what sort of liability risk hospitalists face has been largely undefined, and so we obtained some data from a liability carrier database to try to answer this question. The conventional wisdom seemed to be that hospitalists would be at a relatively high risk of malpractice claims, because they have only relatively brief physician-patient relationships, and because there is the risk associated with the transition of care back to the PCP, such as incidental findings requiring outpatient follow up.
We found that the rate of malpractice claims against hospitalists was actually less than one third the rate of claims against non-hospitalist internal medicine physicians. The rate of claims against hospitalists was 0.52 claims per 100 physician coverage years, as compared to non-hospitalist internal medicine physicians, who had a claims rate that was significantly higher, at 1.91 claims per 100 physician coverage years. The severity of injury in the claims against hospitalists was high, with 50.4% of those claims involving the death of the patient.
Q: To help clarify an issue our readers will likely raise, how did your group classify a hospitalist when scouring the data, especially since we as a specialty can’t unify around one definition? Did all the claims actually use the term hospitalist?
Schaffer: We defined a hospitalist as an internal medicine physician that spends greater than 50% of his or her time practicing in the inpatient setting. The claims did not necessarily use the term hospitalist.
Q: You noted additional claims against hospitalists in the communication and transition of care domains, as well as more treatment (versus diagnosis) actions. Can you elaborate?
Schaffer: When we looked at the types of allegations made in the malpractice claims against hospitalists, we found that a plurality of claims, 41.5%, were for errors in medical treatment, whereas 36.0% were for errors in diagnosis. This was interesting to us because prior literature looking at the types of claims made against PCPs has found that diagnosis-related allegations are the most common type of allegation made in malpractice claims against PCPs, ahead of treatment-related claims (see, for example), So this is one important way in which claims against hospitalists and PCPs differ. Our data do not allow us to answer why hospitalists see more treatment-related claims and PCPs see more diagnosis-related claims. One possible explanation is that, because most patients come under the care of hospitalists after undergoing evaluation in the emergency department that this initial evaluation helps generate diagnostic possibilities and data that make it less likely that the diagnosis will be missed once care is assumed by the hospitalists. However, this is only one theory to explain our data.
Hospitalists generally recognize that transitions of care and communication are areas that are high risk in terms of medical liability and patient safety. Our data support the need for hospitalists to remain focused on these areas, as 37.9% of the claims in our study involved issues with communication and transitions of care.
Q: I have concerns about the evolving nature of hospital medicine and the limited swath of data you analyzed in the 1997-2011 period. You seemed confident claims against hospitalists did not exceed other inpatient practitioners. Also, the number of claims you used to calculate the claims rate was 16 (table 2). Do you feel you captured a representative enough sample?
Schaffer: The number of hospitalist claims used in calculating the claims rate against hospitalists does indeed appear modest, at 16. However, I think the most relevant number in assessing the generalizability of the claims rates presented in our study is the denominator, which is the number of physician coverage years. The number of physician coverage years represents the volume of clinical experience being studied to arrive at the claims rate. The number of physician coverage years we studied for hospitalists was substantial at 3060. The fact that the number of actual claims against hospitalists was low, at 16, was due to the low claims rate for hospitalists, which is what we were trying to ascertain in the paper. Most of our conclusions are based on a database that includes roughly 30% of closed claims in the U.S., and so I would expect that our conclusions should be fairly generalizable.
Q: How do you think a liability company writing policies would interpret your data? Would they be swayed?
Schaffer: I think our data should allay concerns that hospitalists will face a higher claims rate than other internal medicine physicians, though I would be surprised if it influences the premiums paid by hospitalists. Based on our findings, I think it would make sense for liability carriers to have a separate category for hospitalists to be used for internal data collection, since our study suggests that the liability environment for hospitalists may be different than non-hospitalist internal medicine physicians.
Q: Where does your work go from here and any final thoughts for readers?
Schaffer: An area that can be challenging to get at, but that I hope to explore, is what factors predict that a physician may be at elevated risk of a medical malpractice claim. Aside from medical specialty (see, for example), there is not much data about this issue. Knowing what factors put a physician at increased risk of a medical malpractice claim might inform efforts to reduce the risk of malpractice claims against a physician, and, more importantly, enhance patient safety.
Thanks so much for your time, Adam. The hospitalist community looks forward to your follow-up explorations.
About Dr. Adam Schaffer MD
Adam Schaffer, MD is an instructor at Harvard Medical School and an attending physician on the Hospitalist Service at Brigham and Women’s Hospital in Boston. He earned his medical degree from the University of Pennsylvania School of Medicine in 2000 and completed his residency in Internal Medicine at Columbia-Presbyterian Medical Center. Dr. Schaffer also completed a fellowship in Nephrology at New York Presbyterian Hospital-Weill Cornell Medical Center. His academic interests include, in addition to medical malpractice, nephrology and perioperative medicine.
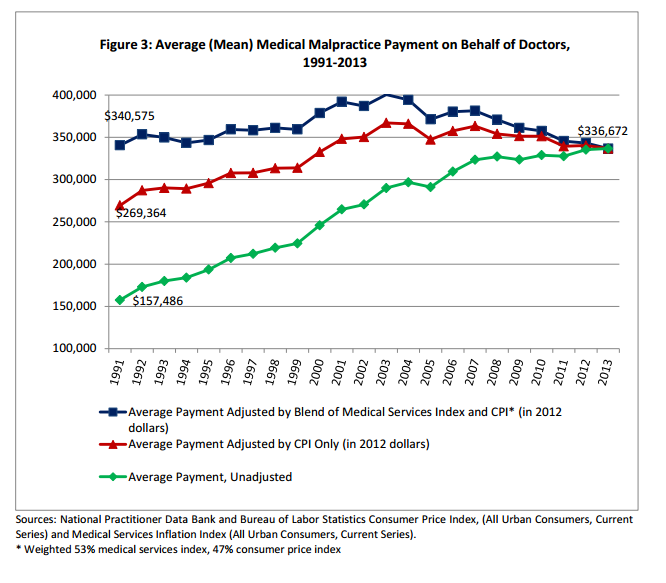
BONUS: A nice update from Public Citizen on med mal payouts in 2013:



[…] In part II, I will introduce you to someone who can shed some light on my original question in the header. I will serve the entree next week, so stay tuned. I hope you enjoyed the amuse bouche. […]
[…] Leader, asks whether hospital-based doctors get sued more often. There’s a follow-up part two that you’ll definitely want to read (hint… that’s where the answer to the […]