by Dr. Luke Hansen MD, MHS
“Why can’t everyone just do the right thing?” is a central question in American healthcare. Providers ask it of patients continually and increasingly in the era of the Triple Aim it is also a question the healthcare system is asking itself. How does one of the most advanced evidence production enterprises in the world nonetheless often fall short when it comes to evidence implementation and health outcomes?
One answer may lie in another commonly heard question in healthcare settings: “When is our next conference call?” American healthcare, like other industries dependent on communication, relies heavily on technology to help create virtual meetings to pursue the goal of collaboration and improvement. Unfortunately, as many of us whose work involves e-collaboration know, these virtual meetings often face barriers to effectiveness unique to their impersonal format.
Over the last five years, we have been engaged in a statewide effort in Illinois to disseminate best practices related to hospital discharge—Project BOOST (Better Outcomes by Optimizing Safe Transitions). BOOST is an evidence-based, multidisciplinary and comprehensive program focused on reducing readmissions by providing expert physician mentoring to improve the discharge transition process, enhance patient/family education and satisfaction, and improve the flow of information among inpatient and outpatient providers. The effort in Illinois is a unique partnership among payors and providers, supported by both Blue Cross Blue Shield of Illinois and the Illinois Hospital Association (IHA), as well as Northwestern University. Between June 2011 and September 2014, a total of 36 acute-care hospitals and 4 long-term acute-care hospitals participated in the Illinois BOOST collaborative.
A distinctive aspect of the BOOST Illinois collaborative is face to face engagement of hospital sites by physician mentors at site visits as well as face to face engagement among sites at the project’s kick off and reunion conferences to foster collaborative learning. Hospitals are assigned a physician mentor who provides teams with content expertise and coaching throughout a year-long quality improvement project engagement. Teams are introduced to their mentors at a kickoff meeting and communicate with mentors via phone monthly. Mentors conduct two face to face site visits, which help teams navigate barriers and elevate the visibility of their work within their organizations. These mentored activities are supplemented by a series of required webinars as well as each site’s own internal group meetings. The collaborative concludes with a reunion conferences to reinforce collaborative lessons learned.
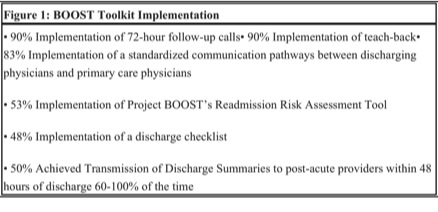
Over the last three years, mentors in Illinois have completed 257 mentor calls and 78 site visits. BOOST sites report high rates of implementation of best practices around transitions of care (See figure 1).
The Illinois collaborative employed multiple face to face experiences as a complement to regular monthly teleconferences between mentors and individual sites, based on our belief that face to face encounters with advisors would be most likely to reveal local contextual components are key to successful adoption of complex clinical delivery systems such as high quality care transitions. However, as technology evolves we also expect increased options for conferencing. While these high-tech alternatives can save time, money, and energy, do they really help programs create sustainable relationships, trust, and collaboration?When asked to rate BOOST elements they found most beneficial, sites consistently emphasize the importance of the face to face aspects of their BOOST experience. On a scale of 1 (“not helpful”) to 5 (“extremely helpful”), site visits and reunion conferences were rated highly at 4.6 each, while and mentor calls were rated at 4.7. Furthermore, participants expressed a desire for additional and ongoing collaboration, requesting “more collaborations with other institutions…” and “more meetings with other members.”
Our experience informs our belief that the face to face component of our intervention is key to success.
Our belief is supported by others who study business communication. Lavallee found that “high-touch promotes trust, a critical component for motivating participation. It helps identify topics of greatest importance to the study as well as elucidate opportunities to disseminate research findings effectively.”1 A “high-touch” program is a traditional approach involving direct contact with participants. Through the process of shared stories, sites develop trust for one another leading to greater engagement and spread of valuable insights. Further, according to Susan Adams, a columnist at Forbes Magazine who has studied teleconference communication versus face to face interactions, “meeting face to face does three things better than virtual meetings, it captures trust, it inspires positive emotions, and it builds relationships.”2 When hospital teams are brought together at reunion conferences it provides a setting for group reflections, cross-communication, and shared learning. A study in the Journal of the American Board of Family Medicine found that when groups are able to reflect collectively on their experiences, teams are able to take back to their organizations key messages and strategies that would benefit them the most.3
Delayed uptake of clinical practices as relatively straightforward as aspirin therapy following myocardial infarction has been lamented for decades, and more recently healthcare improvement efforts have identified similarly delayed implementation of high quality systems and organizational practices. Challenges present in efforts to change complex organizational practices, in contrast to changing individual providers’ clinical practices, include the need to engage diverse stakeholders and account for interpersonal dynamics and organizational culture. We believe that improvement approaches that spend the time and money to bring together clinical sites and implementation experts in face to face interactions are most successful in improving quality and disseminating best practices.
References:
1. Lavallee DC, Wicks P, Alfonso Cristancho R, Mullins CD. Stakeholder engagement in patient-centered outcomes research: high-touch or high-tech? Expert review of pharmacoeconomics & outcomes research. 2014;14(3):335-344.
2. Adams S. “Why we need to meet in person”. Forbes. Feb 2011.
3. Shaw EK, Chase SM, Howard J, Nutting PA, Crabtree BF. More black box to explore: how quality improvement collaboratives shape practice change. The Journal of the American Board of Family Medicine. 2012;25(2):149-157.
Dr. Luke O. Hansen MD, MHS is an Assistant Professor in the Division of Hospital Medicine at the Northwestern University Feinberg School of Medicine. In addition to his clinical practice in hospital medicine, he participates in hospital quality and safety activities as a Unit Medical Director and conducts research in care transitions for older adults. He has been a hospital mentor for the Society of Hospital Medicine’s Project BOOST (Better Outcomes through Optimizing Safe Transitions). He is a member of the Executive Council of the Northern Illinois Chapter of the American College of Physicians.



Leave A Comment