My wife and I are planning to add square footage to our house. We want more space. We are considering an office expansion, a guest room, and making the master bedroom more master and less bedroom. The kids are growing, the family is always visiting, and we have no plans to relocate.
We also need more space for our stuff.
“Everybody’s gotta have a little place for their stuff. That’s all life is about. Trying to find a place for your stuff.” — George Carlin
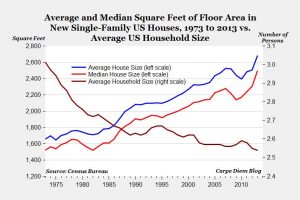
We added a shed, stuffed the closets, and overloaded the garage. How did we get so much stuff? The average US household has 300,000 things in it. In addition, houses in the US have tripled in size since the 1950s, yet fewer people live inside these homes. We’re one of the 25% of American households that have a two-car garage but don’t put both cars in there.
The hospital? That’s different. Our workhouse is a space built for efficiency and streamlined care. Everything in its space, like a giant Code Cart with every drawer perfectly packed, the hospital is a macrocosm of that 3 x 4 feet world that contains all the essentials to resurrect the patient.
Right?
The hospital doesn’t appear to be immune to more stuff. We learn Lean, yet are part of an industry with 30% waste. Overutilization is part of the waste discussion, but I’m also talking about bloat. The parts that are administrative, include failure of care delivery and care coordination, and additions without redesign. Watching hospitals add equipment, spaces, and resources with few design principles are like seeing my toddler do an art project. She simply splashed on more color and paint because she could.
Recently, I was at a hospital where the patient thanked the doctor for ordering the “calf massager”. She felt so much better. Her roommate chimed in as well and asked how she can get one at home. The doctor walked out of the room wondering when the compression devices were ordered for a patient that’s been walking the hallways and was due to leave 24 hours after admission. A look down the unit revealed the next bed, and the next room, and throughout the unit, compression devices attached to the foot of each bed. These leg squeezers are warranted on a small number of inpatients, yet there they are on 100% of beds, and hence most of those patients, even if not ordered by a clinican.
I’ve seen a similar pattern with telemetry. The number of available beds with telemetry seems to be climbing. This is helpful to reduce moving patients around the hospital, from telemetry to medical and back if needed. I’m a proponent of universal beds. Yet, adding more monitored beds without a strategy to reduce overuse is adding waste. Twenty to 50% of telemetry usage may be unnecessary. We see the same with imaging: more machines mean more tests, and not simply improving workflow. When I’m at a buffet, I eat more food. The same applies here.
ERs get more beds to improve capacity. Yet, with often missing the opportunity to implement system redesign to reduce unnecessary admissions, improve access to primary care, reduce length of stay in the hospital, or otherwise reduce inpatient capacity. The bottleneck forms.
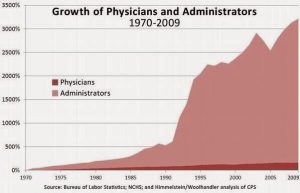
We talk Lean, and then order the fatty porterhouse. We know redesign but instead, add more space. We have regulatory requirements that add to the culture of more not less. More antibiotics, more compression devices, more nursing, more case managers, bigger lobbies, bigger ERs. The only thing that hasn’t grown is the number of doctors! This graph shows the comparative rocketing rise of administrators in healthcare.
So about that addition to the house. I may not be going into the world of Magic Tidying, but we need to declutter before we add on. And that is what we ultimately decided to do. We adjusted our lofty goals for our house remodel. We are spending more on redesign than adding new space. We reconfigured our bathroom and closet to be more functional than adding on new square footage in the master bedroom.
Redesign. Restructure. Remove waste. At least that Lean training worked for the home.
Less is more.



Leave A Comment