I opened the most recent copy of NEJM with anticipation. At last, a review on severe alcohol withdrawal. Perhaps a solution to the age old conflict between psychiatry (start benzo on Monday, decrease by 20-25% daily and discharge on Thursday or Friday) versus medicine (start benzo on Monday, and if they look like a rose on Tuesday, send them home). No such luck.
I did find this though:
“The doses needed to control agitation and insomnia vary dramatically among patients and can be prodigious (e.g., >2000 mg of diazepam in the first 2 days in some patients); this underscores the advisability of providing treatment in a hospital, preferably in an ICU.”
UM. You think?
The management of alcohol withdrawal dangles out there. Not since the CIWA scale (>10 years) has anything new crossed our path. Not a lick. The treatment sits at an intersection between medical, psychiatric, and social domains–and defies our uniform ability to categorize discharge readiness or safety. We use our best judgment and hope to mirror each other’s practice within 2 SD’s.
I am waiting for the SHM plenary in which a resourceful group presents some compelling, new data–and moves the evidence base further down field toward the goal line. Its’ been a long time since we’ve altered practice or learned something new.
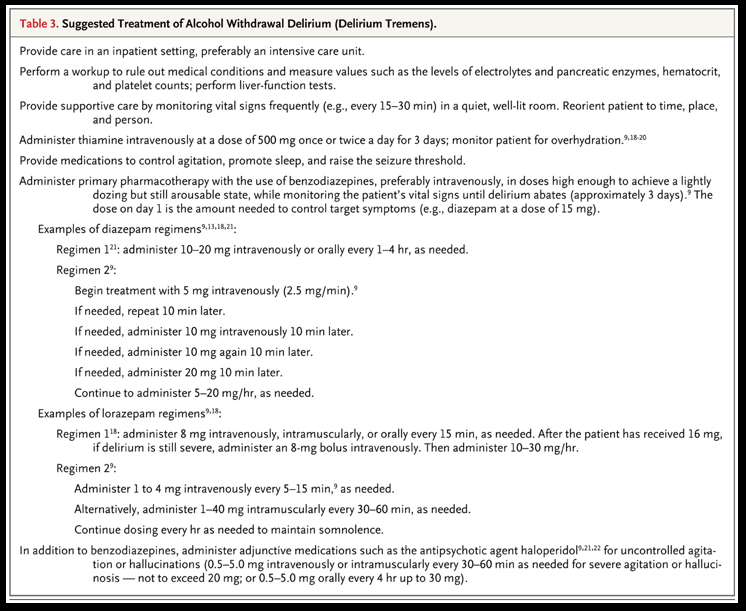
Here’s a handy little table. And yes, it still looks the same:


Leave A Comment