 by Christopher Moriates, MD
by Christopher Moriates, MD
Author of Understanding Value-Based Healthcare*
The hospital chargemaster has become nearly a household term, following its turn as the villain in highly publicized features in Time magazine, The New York Times, and the The Daily Show. Nobody seems to like the chargemaster. But what exactly is it and how does it relate to hospital costs?
The first step is to understand basic hospital accounting terms including “costs,” “charges,” “prices,” and “reimbursement”:
Figure from: Moriates, Arora, Shah. Understanding Value-Based Healthcare. New York, New York: Mcgraw-Hill, 2015.
The chargemaster (also known as the charge description master or “CDM”) is the list of charges for the tens of thousands of billable items at a given hospital – sort of like a menu at a restaurant, but one that is very long and includes reams of inscrutable acronyms and abbreviations. The chargemaster contains the itemized charge that goes on a patient’s bill. This is the amount of money that a self-pay patient is asked to pay for a medical service.
In addition, the chargemaster is generally used as a starting point for closed-door bargaining with different commercial insurers. It is theoretically meant to relate to both actual hospital costs and payments, but it fails miserably at this function.
A study commissioned by the Medicare Payment Advisory Commission (MedPAC) found healthcare delivery systems’ decisions about how and when to apply mark-ups to the actual costs on the chargemaster varies widely based on an array of idiosyncratic factors. Even worse, many hospitals do not have a strategic process for regularly reviewing their charges and some have even lost track of exactly how certain charges were historically determined.
The tale of the chargemaster gets even more gruesome when considering just how big those mark-ups may be. The Centers for Medicare and Medicaid Services (CMS) compiles information annually to determine the ratio of what a day in the hospital costs (operating expenses) by what the hospital charges, called the “ratio of costs to charges” (RCC). These calculations are admittedly imprecise, but are frequently used by hospital accountants and health service researchers as a basis for estimating the costs of providing care. Over the last 20 years, the average hospital RCC has nearly doubled. Charges are now marked up to more than 300% of their estimated costs.
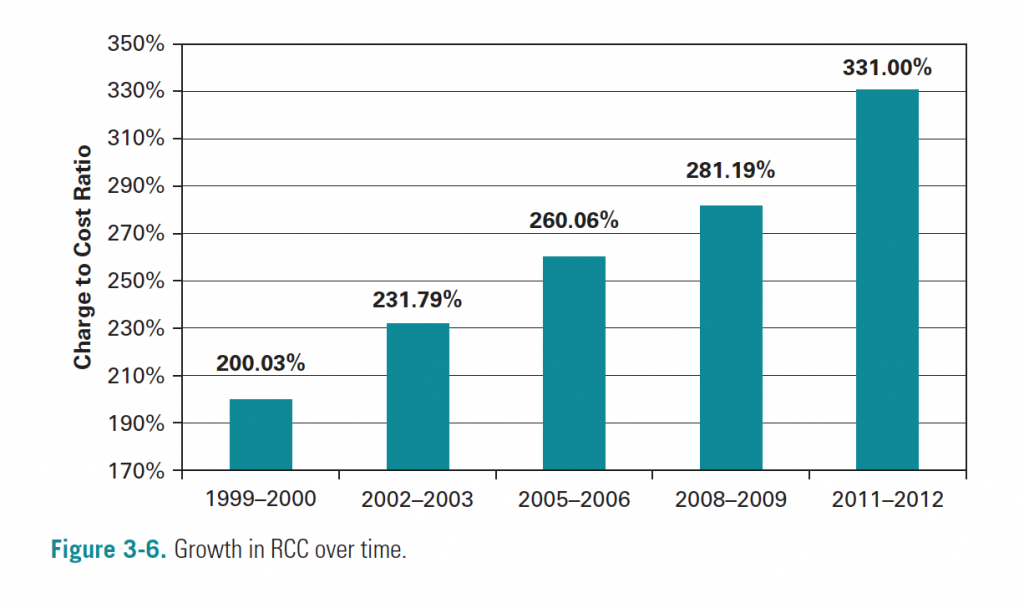
Figure from: Moriates, Arora, Shah. Understanding Value-Based Healthcare. New York, New York: Mcgraw-Hill, 2015.
Some of you are thinking, well, nobody actually pays these charges so what difference does it make? For starters, here are 24,000 words that illustrate just how these charges have affected real patients. Hospital administrators may be quick to defend charging practices, partially by pointing out that charges “rarely reflect what [hospitals] are paid.” Yet, isn’t that exactly the problem? Do we really believe that there isn’t a better way to account for true costs and the uncompensated care delivered at hospitals? Even if patients rarely pay charges, it perpetuates opaque pricing, and in the era of increasing consumer-driven health plans and out-of-pocket costs for patients, opaqueness will not stand.
As a hospitalist, I don’t set the prices on the chargemaster. I am guessing you don’t either. However, hospitalists can advocate for a more rational hospital pricing system and can help shine a light on hospital costs. A first step may be supporting systems that provide full transparency to patients – an example of this is Dartmouth-Hitchcock Medical Center, which has created an “Out-of-Pocket Estimator” for patients.
As for determining true hospital costs, this is challenging. One way is to directly observe each clinical process and determine the time involved in completing each task, assigning a per-minute cost for personnel, space, equipment and administrative overhead. This is not impossible, but it is a lot of work, and it seems few provider organizations are willing to put in this kind of effort if they don’t have to. However, some leading organizations are now creating “cost masters” that reflect the actual costs involved in delivering care. Hospitalists should join in the chorus demanding that hospitals adopt these accounting methods and provide transparent costs to the public.
In addition, we may be able to help deflate bills simply by cutting out as much as a third of the line items through avoiding unnecessary care and overuse.
Will hospitalists help slay the wicked chargemaster?
I (and our patients) sure hope so.
Christopher Moriates, MD is a hospitalist and assistant professor at the University of California at San Francisco, Director of the Caring Wisely program for the UCSF Center for Healthcare Value and Director of Implementation Initiatives at Costs of Care. He co-authored the book Understanding Value-Based Healthcare (McGraw-Hill, 2015), which Atul Gawande has called “a masterful primer for all clinicians,” and Bob Wachter said is “essential reading for everyone who care about making our system better.”
*This post is part of a series for The Hospital Leader blog highlighting topics or lessons from this book. Stay tuned for more on value-based care from Dr. Moriates.




There’s another key component to chargemaster pricing that you don’t reference at all.
While the odd Saudi billionaire may well fly in and pay inflated chargemaster pricing with gold bullion – most American citizens certainly won’t. But that doesn’t mean it doesn’t serve a large accounting function – tax deductibility.
It’s another big, opaque component to healthcare – but taxation (in all forms – for-profit, not-for-profit, and non-profit) plays an enormous role in our $3.2 trillion NHE. The larger you can make a figure for legitimate tax deductions – the more it can offset other forms of revenue as income.
Dear Dan – Thank you so much for your comment. This is an important point that you make, both about the function of the chargemaster for the “Saudi billionaire” — a real phenomenon that we see at large academic medical centers like ours, particularly when considering things like liver transplantation — and as a basis to justify large tax deductions and claim an incredibly inflated amount of “charity care.”
There are many tentacles of the Chargemaster that can be examined and dissected. Thanks for helping us do so.
Sincerely – Chris
Excellent points. I never understood about chargemasters before as I understood with this article and comments.
-Founder of http://www.BecomeAHospitalist.com
To be consistent with Fig. 3-6, wouldn’t RCC be “ratio of charges to costs” not what’s stated in the article: “ratio of costs to charges”. Let’s not further confuse readers who have enough trouble understanding the black arts of medical bills.
Well written post, Chris.
I think one important factor in the markup of costs is that ether is no standardized methodology to estimate costs accurately. While some costs like (medications, room, …) could be easily determined, others like time and service charges could vary widely among organizations. I agree that we Hospitalist could play a major role in reducing costs.
Interesting point by Tony about RCC, using “charges to cost” for the purposes of the post might help understand the data and the article better..
Thanks.
Rupesh.
On Google trends, the terms hospital medicine and hospitalist seem to have flattened — so indeed, perhaps we have arrived.