Regulation always seems like a good idea when the other person has to comply. I know a lot about healthcare, but no so much about energy, education, or food service. Despite my knowledge gap, if a rule goes into effect requiring an individual or company to reduce carbon emissions, add classroom time, or post calorie data, who am I to complain. Someone thought the regulation through, vetted the perspectives of all constituents, and weighed the benefits and harms. Most of us will live a bit better or safer due to the efforts of well-intended public officials. Right?
When you begin to pay attention to your patch however, you realize the gripes you have about your regulations (because bureaucrats only scrutinize me) differ little from others as they confront theirs. Your perspective expands and allows for a more measured stance when you say, encounter proposals in the papers or journals. You begin to question potential impositions (not intentions) and cogitate more clearly on how best to utilize limited resources in bringing a desired result.
To wit, for those who work in hospitals, you will recognize the following:
Effective January 1, 2011, the Patient Protection Affordable Care Act, through a Final Rule released by the Centers for Medicare and Medicaid Services mandates that a patient’s eligibility for the Medicare Home Health benefit relies upon a documented face-to-face encounter between a patient and physician (or other approved practitioner) for the clinical reason that home health services have been ordered.
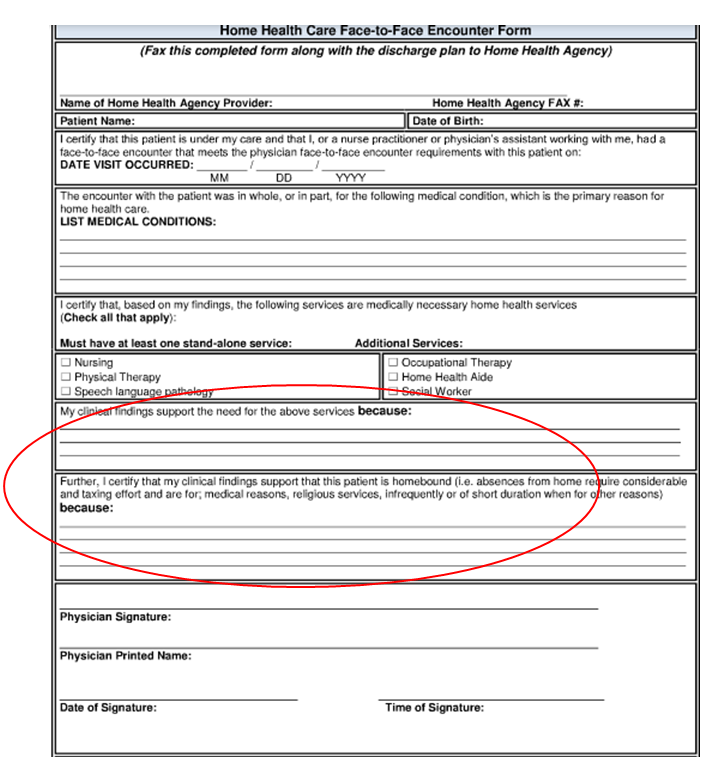
Yes, face-to-face. For those unfamiliar with the face-to-face document, as of 2011 all patients requiring a skilled service at home (PT, nursing care) need a provider signed form attesting to the patient’s need for the same. For example, if the patient has profound weakness, a complex wound, or poor vision, we must indicate the disability so the home agency can begin support. No form. No service.
Everyone working in a hospital delivering acute services knows the face-to-face. The document has become a daily ritual.
However, soon after the face-to-face introduction, we became inured with the process and the signature itself, not whether the investigation of appropriateness, e.g., 2, 4 or 6 weeks of visits, has become the objective. The case manager, “the discharge quarterback,” shovels the forms, scribbles in the indication—see the red circle above—and we sign.
A novice might question the proceedings, but speaking with others and from my own experience, if the physical therapist says the woman with Parkinson’s disease needs “x,” or the wound care specialist states the diabetic amputee needs “y,” we agree.
All of us have become excessively busy caring for our patients. We prefer to engage in the tasks they value most versus expending mental energy on distractions. Distractions most of us feel ill-suited in ordaining incidentally.
(I often wonder who enlisted us as the ancillary service police. Maybe I wonder too much).
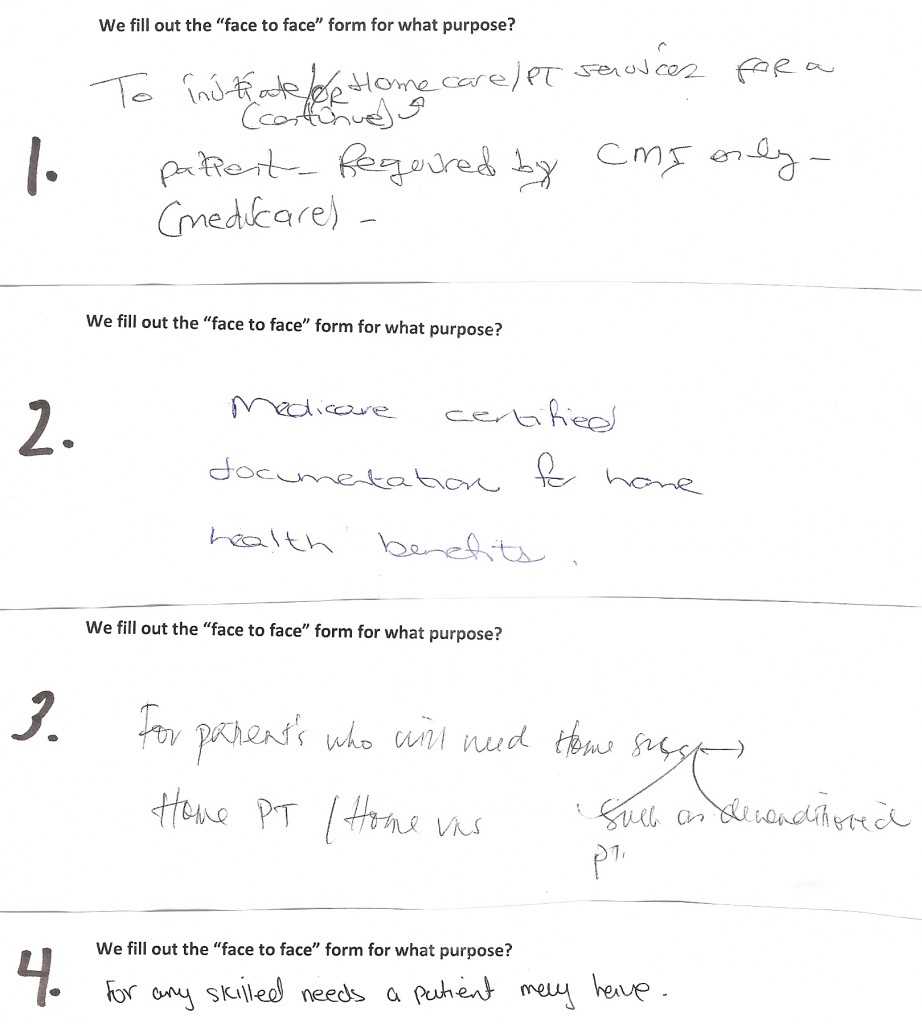
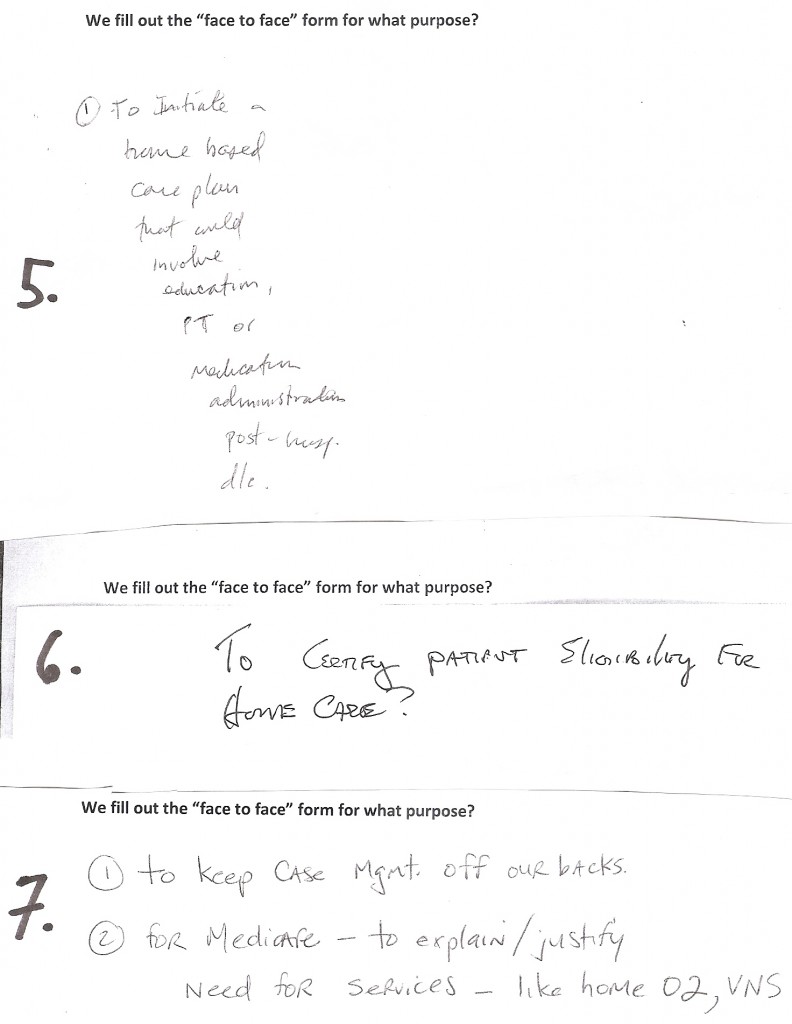
Curious as to how anesthetized we have become, I asked my colleagues why ward personnel request our John Hancock on discharge day. Rather than me tell you, have a look at the sampling:
I cannot verify whether they looked up why (I think some did), but I would be willing to bet response #7 captures the spirit most inpatient providers exude when engaging the document. Regardless, the aggregate score for my sampling of answers would be a B minus. A higher score would necessitate more of #2, and less of the “need skilled care” vagaries of the others.
Interestingly, the discharge staff may be more confused. In casually speaking with them, many could not convey whether the state, local insurance companies, or Medicare require the form. As one said, “we just push the paper, don’t ask me!”
I do believe most folks could not articulate who (CMS) and why (waste and fraud) we have the regulation. Local factors such as demands of individual agencies, i.e., “you must sign now”—and not the 24 hours allowed, and how the document moves through organizations, distort the intent of the instruction.
Lest you think I am needlessly carping, the last two years working with the face-to-face form has been a lesson in what can go astray with bureaucratic directives.
I know why the form exists. I know the intent of the individuals who brought about the process. I also know CMS personnel bring passion and dedication to their jobs and do not lack intellect (trust me, go visit).
However, the promise of health reform and the trickle down message of patient-centeredness; the attempts at improving provider efficiency and economizing our time; and aligning the right job with the right people (or whether the job needs doing at all), seems like a tall order when faced with a hollow form. If we have to expend intellectual capital, we want to make it matter.
I don’t believe the face-to-face form has saved appreciable dollars or landed any fraudulent service providers in jail. Prove me wrong.
In the trenches, these types of activities take their toll. We do not need more cynics–especially in an environment undergoing rapid change with discouraged workers. If I want cynics, I can watch C-SPAN.
ADDENDUM: A colleague writes (and HH= home health):
You’ve captured the essence of rulemaking and its pitfalls quite well. Your example of the face-to-face is also really interesting in that it really demonstrates how certain facets of healthcare can take a rule and turn it into something somewhat more or less than the intent. From first hand, I can say that CMS does not require a ‘signature’ form for the F2F encounter and doesn’t necessarily want a form to be used (from direct conversation w/Jon Blum). Also, to quote CMS directly, “CMS does not require a specific form for face-to-face documentation…”
HH has actually been the pusher of the form and what you are signing is probably actually theirs or something they asked the hospital to adopt. Regardless, you’ve shown how a well intended rule to help prevent fraud is really just an additional hurdle to sign off on – or from the HH perspective – gather. And how the mechanics end of defeating this purpose.


[…] Posted at The Hospital Leader on […]