“One-out-of-three”. I’m going to say that one more time: “One-out-of-three”. That’s the amount of medical resources that a group of surveyed hospitalists believe is used toward defensive medicine. Can you think of any other aspect of your life in which 1/3 of your decisions are made, not to optimize the outcome, but “just to be safe…”?
For the life of me, I can’t…
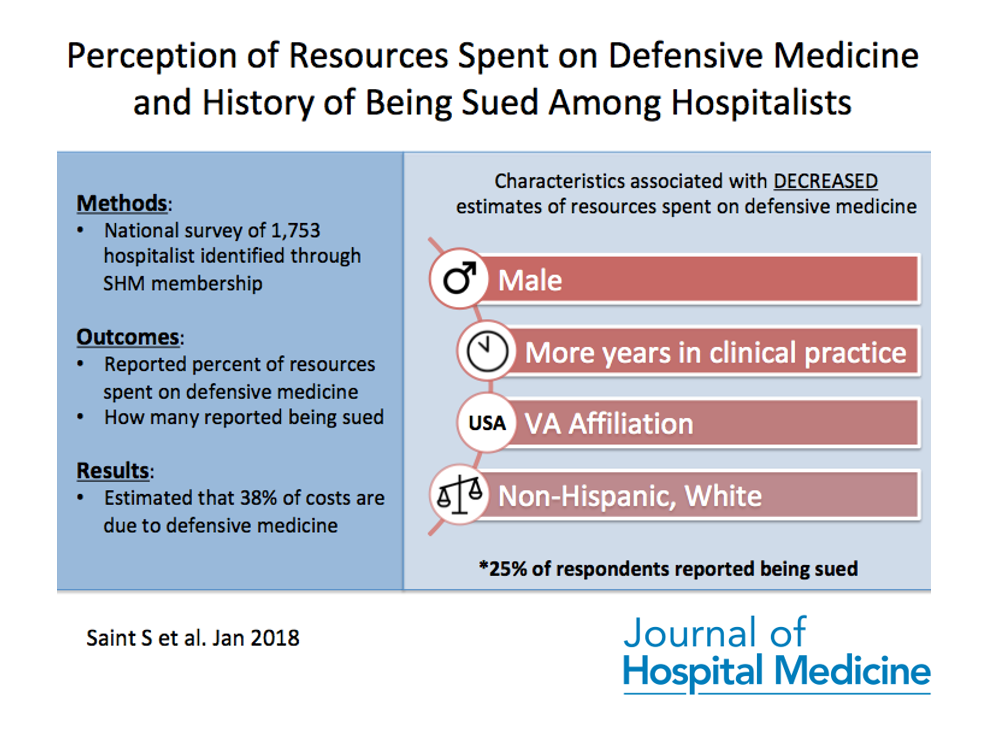
A group of researchers at the University of Michigan recently surveyed over 1,000 hospitalists throughout the country to assess their perceptions of how much we hospitalists spend on defensive medicine. They also looked at how many hospitalists reported being sued and whether this was tied to their estimates of defensive medicine (turns out it wasn’t). What they did find, was that surveyed physicians believed ~38% of healthcare costs are due to defensive medicine and that 25% of those surveyed also reported being sued.
While not frequently reported in hospital medicine literature, this topic remains highly salient as it affects the health care system to the tune of ~$56 billion dollars/year! Even if you’ve never been the subject of a malpractice lawsuit, this study begins to explore how the simple threat of litigation may influence your ordering patterns. Some other food for thought:
- The investigators reported that VA-affiliated practitioners estimated a lower percentage of defensive medicine (32% vs. 38%). To me, 32% still feels high. Why? Well, because as the authors explain, VA physicians (for which I am one) are sheltered from direct liability through enterprise liability. One might assume that under these circumstances, defensive medicine might be a lot less than 32%. But maybe I’m being too optimistic. Also, see #3 below…
- Are there alternative methods to the current malpractice system? While tort reform and damage caps have not been shown to decrease the practice of defensive medicine, an idea, termed the Patient Compensation System (PCS), has emerged as one alternative to our current system. Under PCS, physicians and hospitals would no longer be sued for malpractice. Instead, hearings would be held in front of a panel of health experts, and – should they find that a medical injury was preventable, the patient would receive compensation. One study found that such a system could cut medical expenses by $7 billion/year in one state alone.
- Even if we get rid of malpractice, will this actually change the way we practice? A RAND-sponsored study in NEJM in 2014 makes the argument that “…malpractice reform may have less effect on costs than has been projected by conventional wisdom”, per lead author Daniel Waxman. In their study, legislation in regulating malpractice in 3 states had no effect on imaging rates, average charges, or hospital admissions.
There’s certainly a lot more to unpack on this subject, and we’d love to hear your thoughts and experiences. Join my colleague Vineet Arora, MD (@FutureDocs) with guest authors: Sanjay Saint, MD (@sanjaysaint), Vineet Chopra, MD (@vineet_chopra) and Allen Kachalia, MD, JD (@allenkachalia) on Monday, February 26th at 9PM ET where we will discuss “Perception of Resources Spent on Defensive Medicine and History of Being Sued Among Hospitalists: Results from a National Survey”
Not familiar with #JHMChat? Since October 2015, JHM has reviewed and discussed more than two dozen articles with many focusing on improving the value and quality of care we provide to hospitalized patients. Medical students, residents and practicing hospitalists are encouraged to join, as we discuss a broad array of topics that affect the care of the hospitalized patient. It’s a great opportunity to meet others, learn and even earn free CME.
To participate, just type “#JHMChat” in the search box on the top right corner of your Twitter face page, click on the “Latest” tab at the top left of the page and join the conversation.



I will do my best to make the JHMChat, but I may not be available at that time, so I wanted to reply here.
I wonder how people would have responded to what percentage of care is spent on defensive medicine is inappropriate? For instance, if people are using the Wells score for PE – that +/- 3 for “is PE the most likely diagnosis” – people who are “defensive” may add 3 and then get the CT, but that does not make the CT inappropriate. If tests are ordered purely to avoid malpractice, then I would consider that inappropriate and perhaps even fraudulent since insurance companies / CMS would be billed for these unnecessary diagnostic services for the sole purpose of “protecting” providers. Additionally, future educational efforts may be helpful in showing doctors how many malpractice claims are based on incidental findings found on “inappropriate” tests (or tests ordered as an inpatient not resulted until after discharge / and potentially not followed up) as a way to help providers see that more is not always better or safer.