By Chris Moriates, MD
“Value” is not synonymous with costs. Don’t let anyone tell you otherwise.
Recently I was asked to provide my thoughts about “a few potential value metrics” at a large academic medical center. The metrics I was sent by this hospital administrator were essentially costs per case and length of stay. In other words, the financial indicators of the hospital system were merely copied-and-pasted under a new banner of VALUE. True that measuring value is complicated and I do appreciate the effort, but I was not about to get out my “hospitalist-approved” stamp.
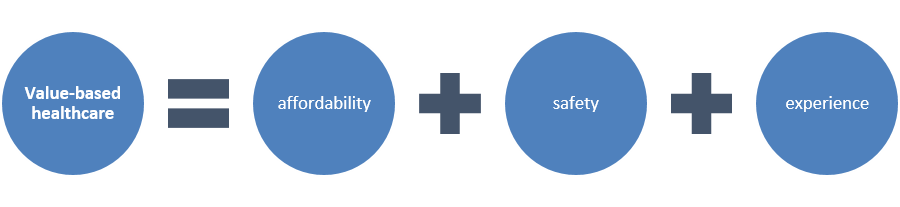
Value may indeed be in the eye of the beholder. In Dr. Lisa Rosenbaum’s brilliant NEJM article from 2013, she contrasts the gulf between desiring, but also applying, value-based principles at the bedside. Regardless, one thing that everyone can agree on is that value must integrate some aspects of quality of care along with costs. To measure a value metric, there should be some sense of desired outcomes per unit cost. To be clear, I do not demure or get squirmy when discussing costs in healthcare – I mean, our McGraw-Hill book “Understanding Value-Based Healthcare” has a picture of a hospital bill right there on the cover. BUT, if value becomes conflated to merely mean cost, we – healthcare givers and patients – have lost everything!
 When we talk about value in healthcare, we are not just talking about pinching pennies. We don’t want “cheap” healthcare, just like we don’t really want “cheap” toilet paper. We want high quality. We want to know it will work and not fall apart when we need it most. But, we also DO NOT want to be gouged. We want bang for our buck. In healthcare, we are currently spending a whole lot of bucks, yet, by essentially all measures, we are not getting a lot of bang. We are buying the most expensive toilet paper in the world, but too often it seems to just fall apart.
When we talk about value in healthcare, we are not just talking about pinching pennies. We don’t want “cheap” healthcare, just like we don’t really want “cheap” toilet paper. We want high quality. We want to know it will work and not fall apart when we need it most. But, we also DO NOT want to be gouged. We want bang for our buck. In healthcare, we are currently spending a whole lot of bucks, yet, by essentially all measures, we are not getting a lot of bang. We are buying the most expensive toilet paper in the world, but too often it seems to just fall apart.
The distinction between cost and value is critical. Certain high-cost interventions are extremely beneficial in the right setting. This past year, I admitted a morbidly obese patient that I suspected to have an epidural abscess. To order her an MRI, I had to coordinate ambulance transportation with a dedicated nurse to the larger MRI scanner across town. The cost of this must have been staggering. And I realized I may look like a hypocrite the next time I stood in front of the interns to teach our UCSF Cost Awareness curriculum.
My patient did indeed have an epidural abscess and required neurosurgical evaluation. I was so thankful that I had access to that MRI. It was of great value for this patient, and probably would have been even if it were negative. However, that same study – MRI of the back – is considered low-value when used for routine evaluation of common low back pain, since it does not improve outcomes.
There are other interventions that are typically low-value, regardless of cost, because they do not improve patient outcomes under almost any circumstances, and even may cause harm. Consider the routine, rather than clinically indicated, replacement of peripheral IVs, which has been shown to provide no difference in rates of infection or phlebitis compared to replacing PIVs only when they have failed or show evidence of emerging infection. Though the individual cost savings from saving plastic PIVs is rather minimal, this practice could likely be completely eliminated without negatively effecting patients. In fact, decreasing needle sticks would be very welcomed by patients and is likely to improve their care experience. Even low-cost interventions may be of low-value and should be targeted for elimination. Therefore, although cost is part of the value calculation, it does not solely define it.
Christopher Moriates, MD is a hospitalist and assistant professor at the University of California at San Francisco, Director of the Caring Wisely program for the UCSF Center for Healthcare Value and Director of Implementation Initiatives at Costs of Care. He co-authored the book Understanding Value-Based Healthcare (McGraw-Hill, 2015), which Atul Gawande has called “a masterful primer for all clinicians,” and Bob Wachter said is “essential reading for everyone who care about making our system better.”
*This post is part of a series for The Hospital Leader blog highlighting topics or lessons from this book. Stay tuned for more on value-based care from Dr. Moriates.




Chris, I so enjoyed your article and am so proud of how you are contributing to right thinking in the medical field.w