My patient was a 69 year old lady with metastatic small cell lung cancer. She was on experimental chemotherapy and was admitted from clinic with worsening lower extremity edema and a new oxygen requirement. She underwent a chest and abdominal CT that revealed new pulmonary masses, tumor and a mass invading her right pulmonary artery, a new loculated pleural effusion, and acute thrombus in the IVC that was occluding her hepatic veins as well as extending into her iliac veins bilaterally. She was tachycardic and tachypneic. Every time she moved, despite supplemental oxygen, she desaturated into the 60 percent range.
OK, pop quiz: What is the answer to this patient management problem?
If you have answered the word “hospice,” you are right.
I spoke with the outpatient oncologist, the palliative care team, and had a meeting with the patient and her daughter explaining the lack of clear therapeutic options. They were in agreement that resuscitation and ICU transfer was not what they wanted; they were amenable to the option of hospice. When I communicated this conversation to the outpatient oncologist his response was “Oh good.” A similar comment was received from the palliative care attending. And as I scurried back to my office to document the conversation and get the DNR order placed, I felt, well, I felt relief.
But then it made me think: Why do I feel relief? Why is every consultant’s response that of relief? “Oh good” being the sort of universal reply. Is it laziness? Once a patient is in hospice care there is no diagnostic dilemma, no determination of a best plan, no active management. We can just put our feet up on the desk and twirl our stethoscopes while we shop online, right? Or, maybe it’s just relief from the stress of trying to push that proverbial boulder up that proverbial hill – that constant salesmanship and manipulation, trying to get a patient or family to see what you see. Or relief from the anxiety, from the burden of worrying about that sinus tachycardia, that respiratory rate, that fever.
Maybe those are factors. But I think the relief response is more likely due to the fact that by the time you bring up hospice, all of the available options have been explored and abandoned. And that so so many patients and their families seem to have unrealistic expectations about their lifespan, despite your very best efforts to demonstrate a realistic arc of their illness. It is a skewed perspective, caring for hospitalized patients. We don’t see the patients who agree to hospice before that hail Mary pass that often ends in a terminal hospitalization. We often only see patients who demand more, who reject reality, who refuse to believe in their own mortality. And we know as providers that more does not really get more quality, or even more life, as many researchers, including an August 19, 2010 New England Journal of Medicine article demonstrate, that patients with non-small-cell lung cancer actually lived LONGER with earlier palliative care.
Finally, I think that relief is a reflection too of the “right path.” If it is right for the patient, then you feel peace with the decision, you feel relief, you feel right. And I hope the patient does too.


First of all, may I suggest that you take the lead in your hospital and transition from DNR to AND – Allow natural death. The conversations with the family are much more comforting – especially in spiritually or religiously oriented cultures – if the provider avoids speaking of not doing anything to allowing nature to take its course. Change the words and you change the conversations and the patient/family’s understanding.
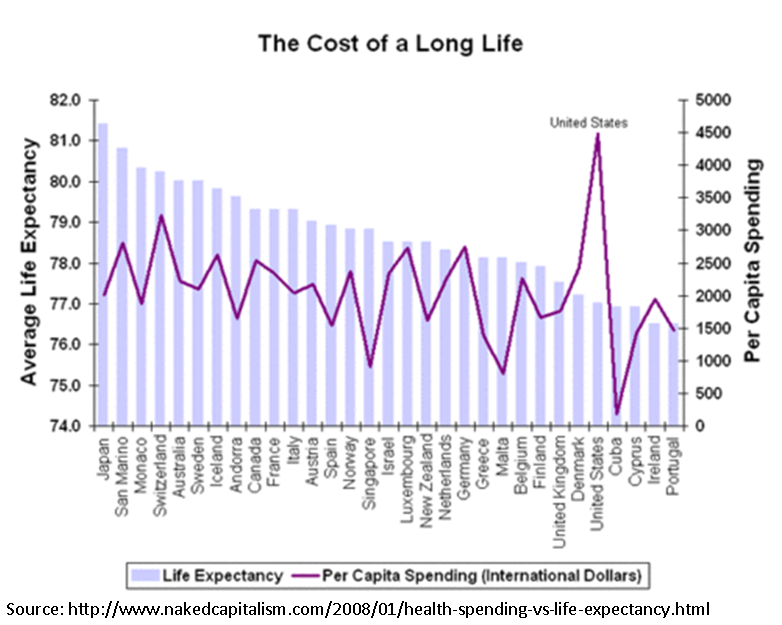
Welcome to the American Healthcare system where we can & will do everything to keep you alive in a Frankenstein-like fashion until your last gasp, quality of life be damned. God-forbid anyone bring up end-of-life issues surrounding cancer or advanced medical illnesses (e.g., end stage CHF, COPD, cirrhosis, etc), palliative care or hospice lest they get accused of being part of a Death Panel trying to kill grandma. I
t’s not just what are we thinking, but what are we DOING to our patients when we give chemotherapy literally up to 5 minutes before a patient with widely metastatic CA dies?
Unfortunately neither American society, healthcare providers in general nor politicians are ready to address this issue & our spending will continue to spiral at an unsustainable rate to the detriment of quality of life in the morbidly ill and dying.