Because hospitalists lack a specialty code for billing (probably forthcoming), and we do not have formal board certification (I would bet it’s in our future), anyone interested in identifying hospitalists beyond their hospital walls has a tough slog. You can call several thousand hospitals and speak with the appropriate department and question; you can call every internist, pediatrician or family practitioner in the AMA database and ask them, “Are you a hospitalist?”; or you can find an alternate method—because the latter two will keep you busy until the next solar eclipse.
Knowing adult inpatient practitioners bill just a small cluster of codes–observation, critical care, or inpatient–having access to a national database with physician billing data (Part B submissions) would provide a route to determine which docs practice in acute care settings.
As it happens, last year CMS released for the first time a motherlode of data (background here). Never before did we have access to physician billing reports from the feds. Now we do. You can even look yourself up.
Moreover, with that data we can determine the nature of the work each doctor performs and also speculate on the nature of their practice. For example, internists and family practitioners billing above a certain threshold of inpatient, observation, and critical care codes (“the cluster”) would likely be a hospitalist. It is just a matter of how we set the boundary. Well, that’s what we did:
Our paper, Updating threshold-based identification of hospitalists in 2012 Medicare pay data, breaks the details down:
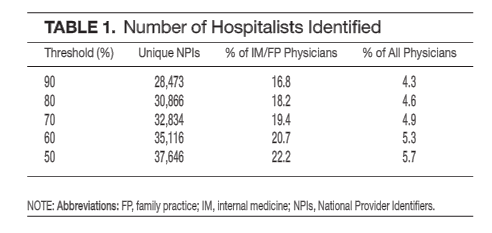
If you set the definition of a hospitalist at a 90% cluster, you can see the absolute and relative values. Likewise, at 80% you see the same–but with greater sensitivity (and perhaps lower specificity) with a commensurate increase in the number inpatient practitioners identified. Physicians billing more than 50-60% of their codes within our cluster would also likely classify themselves as a hospitalist. Nowadays, it would be the rarest of “ambulatory” doctors who have that kind of inpatient productivity. Fifty percent as lower bounds seems appropriate.
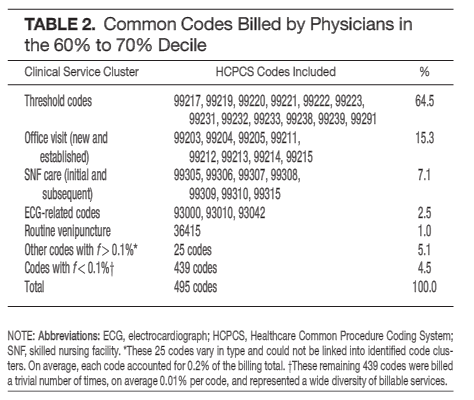
The delta between the fiftieth and ninetieth percentiles comprises ten thousand physicians. If we assume each of those ten thousand works as a hospitalist, what other codes might they be submitting and what is the range of their service? We looked:
Not unexpected, hospitalists perform subacute, ambulatory, and other varied duties, along with their hospital work. A fifth of hospitalists then, probably have augmented skill sets to accommodate their unique practice settings.
So, our findings reveal about five percent of physicians practice hospital medicine. One in five internist and family practitioners do the same. Why does it matter?
Delivery systems will require means to account for, and deploy the proper mix of providers. Hospitalists have and will continue to function in discharge planning, care transition, and post-acute care roles, likely in substantial numbers based on our findings. Absent a unique identifier, health leaders—be they policy makers, hospital executives, or payers, will be ill-equipped to interpret data and apportion resources in an optimal manner.
With better workforce accounting, a firmer grasp of the role hospitalists contribute in team-based care will have positive impacts in several domains. First, comparing groups or systems of care and the mix of providers they use and the outcomes they achieve will contribute to better allocative efficiency. Second, benchmarking and rewarding performance requires information at all health system levels, from regions down to individual providers. Lastly, the means by which we organize care, especially with the federal government expanding its use of bundled or global compensation, requires a more precise reading of who does what. Providers will require fair play; to reward them in an equitable manner necessitates accurate data to inform payers of their work effort and patient service.
The sizable number of discharge and observation codes utilized by hospitalists impacts millions of Medicare beneficiaries undergoing billions of dollars’ worth of testing and referrals. As hospitalists become more responsible for their care, in addition to patients with and without other forms of insurance coverage, tracking resource use will be more than just a luxury, but an imperative. The imprimatur from regulators and payers demands precise and valid data—and given the speed of system change, and the likely effect hospitalists will have, we need a top-down effort to identify them. Bottom line. We require a unique billing code.
I would also add with Physician Compare and reporting of quality performance scores maturing and readying for a full ramp up, and that means risk-based pay, comparing like physicians is a must. Throwing an anonymous group of internists or FPs into one giant matching pool will cause a ruckus. We have to know the practice locale of all providers and determine who does what.
Since the release of our paper, CMS has made 2013 data available. We will take a look and note any changes or unusual findings.



[…] no specific billing code or board certification for hospitalists, so how do you track them down? The Hospital Leader has two suggestions: ask everyone “are you a hospitalist?” or dig deep into the […]