Years ago, I heard the saying, “For you [as a hospitalist], it may just be Monday or Tuesday, but for the patient it is often the worst day of their life.”
This powerful medical aphorism captures the stark differences that can exist between a patient and a doctor. Physicians and health care systems are often chided for not understanding or empathizing with hospitalized patient experiences as well as we could. As a physician (and a father to children who have been hospitalized), this critique is wholly correct…
In an attempt to bring the patient and hospital medicine communities together, we focused our recent #JHMChat on the hospitalized patient experience – centering on the recently published article, “Just Getting a Cup of Coffee – Considering Best Practices for Patient Movement off the Hospital Floor.” While #JHMChat has covered on a broad range of topics over the years, we had yet to engage the most important one – our patients. We were lucky to have Dr. David Alfandre (senior author) and Brooke Vittimberga (a wonderfully insightful individual who has experienced hospitalization through her battle with AML) join us as special guests in our discussion around this topic.
As of this writing, we had >100 participants with >4 million Twitter impressions. While these numbers are impressive, I was most struck by the depth of the conversation and the very personal stories that patients shared. I wanted to use this forum to highlight a few take-home points that were most salient to me. But instead of writing it all out myself, I think it’s best if it comes through patients’ voices:
- Transparency is job #1
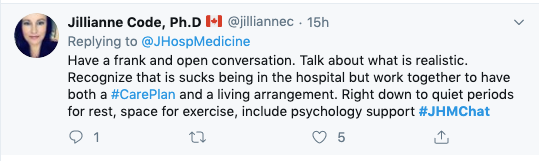
As Dr. Jilliane Code points out, we need to communicate better with our patients. The simple act of (actually!) sitting down and speaking openly and candidly about what patients can expect during the hospitalization is so important (and obviously not done enough). We fail our patients at the point of admission if we do not do this.
But, what I also love about Dr. Code’s tweet is that she mentions what we should expect from her. Are there times of the day that are best to talk? Is he not a morning person? How does she deal with the stress of being hospitalized? While we may not be able to accommodate every patient’s preference, just knowing this information and having this conversation is a great start in recognizing that we are dealing with a human and not a diagnosis. Which takes me to #2…
- Keep the human in mind at all times
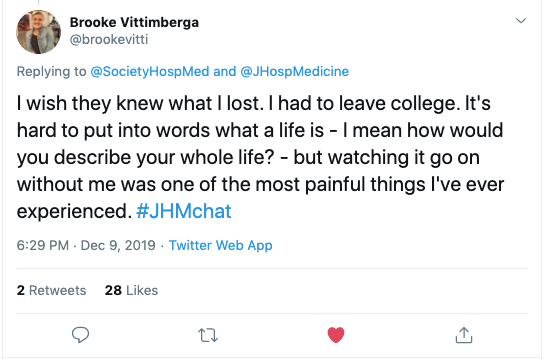
Brooke Vittimberga pointed out that while we often try to understand what a patient is going through while they are in the hospital, it’s important to understand what they’re missing outside the hospital, as well. Our younger patients are often missing out on experiencing life’s milestones (i.e., developing romantic relationships, finding/keeping a job, working on their education) in a way none of us could have imagined. Understanding that there is a human in that bed trying to accomplish the same things we have can’t be stressed enough. We need to view patients as the individuals they are beyond the walls of the hospital and know that they are going through life, just like the rest of us. Recognizing this will bring the humanity back into our care.
- Always give your patient hope
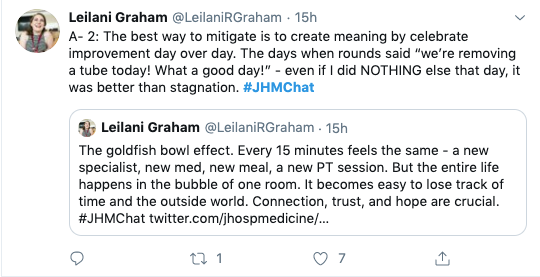
As busy clinicians, we often get lost in the repeated processes of admissions and discharges. We sometimes fail to see that the seemingly small successes (improved labs, completed procedures, progress with physical therapy, etc.) can actually be big accomplishments for our patients. The drudgery of being hospitalized can be mitigated – in part, by finding those small wins and celebrating them with our patients. Leilani Graham saliently points out that keeping hope alive and being open and transparent with our patients (see #1) can be one way we can bring a little positivity to the often negative experience of being in a hospital.
To be honest, there were a number of ‘teachable moments’ in our discussion, and I chose the few that really stood out to me. To all my clinical colleagues out there, I’d recommend you take 5-10 minutes and peruse the discussion here. I think you’ll find some fantastic insights and nuggets of truth that will undoubtedly change the way you practice medicine and interact with your patients.
I’ll leave with one of the final tweets from Dr. David Alfandre whose genuine expression of gratitude captured all of our appreciation for our patient participants.
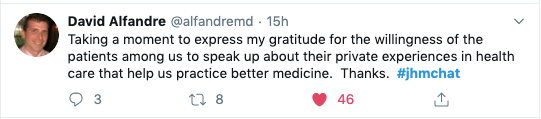
Without their voices and participation, we wouldn’t be able to improve.
If this conversation sounds interesting to you, please feel free to join us for future #JHMChats. We hold them approximately every month and cover a wide variety of topics, from medical education, quality and patient safety, to value-based care. Keep your eyes open on Twitter and follow the @JHospMedicine handle for information on future chats.



Leave A Comment