Economists describe preferences in two ways: revealed and stated. Say, for example, I asked you to implement a penalty program for your team with the goal of decreasing the number of occasions members did not clean their hands after a patient encounter. Because you know bad hands equal bad outcomes, you’re apt to offer up a more than token sanction. Maybe it’s a financial levy or required service beyond the expected, but you will probably suggest a “punishment” that does not quite smart, but imparts just a bit of a sting. Your stated preference.
Nevertheless, as far as hand cleaning goes, although we would want to set the bar high–say 100% of the time, emergencies do happen. We get distracted with both legitimate patient care and personal intrusions. A monitoring system, a good one, might put you at ninety-two percent compliance. Keep in mind a hospital these days hovers around fifty percent or less.
But because of your extraordinary skills, and the justifiable preoccupations of the moment, you would mete out the penalty just on your colleague. She did not have the kind of day you had. You heard from daycare and your kid just vomited, or the intern on the fourth floor just miffed a patient’s family. And because of your specialness, and because you understand the importance of hand hygiene, no penalty should come your way. Stuff happens. Legitimate stuff. The revealed preference.
As I read a terrific blog post by Bob Wachter in Health Affairs, one I agreed with, on the need to direct handwashing responsibility to an individual rather than their affiliated institution, the above kept swirling through my head.
He offered up the following list as qualifying criteria for any process an oversight body deems as “must do” for an individual: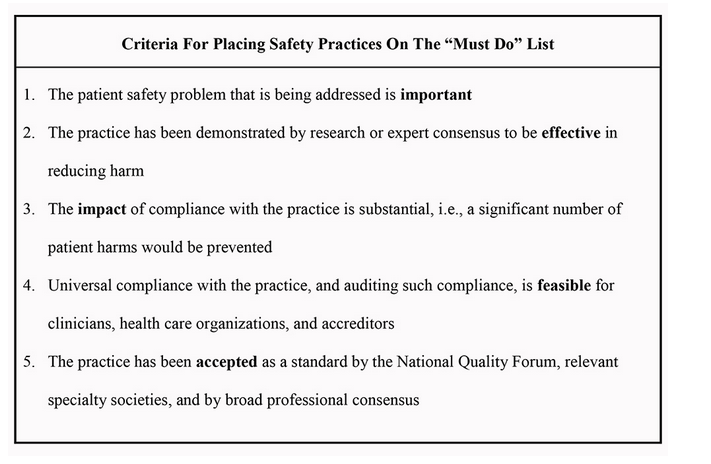
They all look good to me. But I kept thinking about a missing six and seven: 6) specifying the penalty, and 7) identify the manner of monitoring required to ensure a valid rollout with provider assent. They are both intertwined.
An observer who spends three to four hours a quarter on a ward watching providers come and go, in drips and drabs, for example, will not capture a sufficient snapshot of one provider’s performance. Any discipline stemming from a limited number of observations strikes me as wrong.
What options does a hospital have in overseeing compliance? I can think of a few:
1. Use in-house sentinels to observe (with stealth) at random times during the week, rotating from ward to ward. Educate.
2. Use third-party sentinels to do the same.
3. Instill a self-policing culture.
4. A regulatory body makes periodic, unannounced, on-site reviews.
5. Employ technology to monitor compliance in a continuous manner.
6. Use a combination of some or all.
Upshifting from forty to seventy percent compliance probably won’t require more than one strategy–if an organization is serious. However, as an intervention, random, infrequent checks probably will not get the team past the seventy percent mark, give or take. It will also piss a lot of people off based on the inadequate reckoning of their scores. That’s assuming audits won’t be gamed (“we are watching this week folks”), or we can attribute patient harm to a doc’s dirty hand (DNA probes??).
I would also add that paying by DRG weighted episodes, a system not disappearing anytime soon, disincentivizes hospitals from cracking down. Nosocomial infections, not easily traced, pay the bills and keep the lights on. The superior institutions get it, but let’s face it, not every beacon hospital will be preaching four-part harmony to a nationwide CFO choir singing a buff my bill, what’s-in-it-for-me, honky-tonk tune.
Moreover, if we desire report cards on providers–because this is an individual sport after all–we will need to aggregate data based on the totality of an individual’s activity. Gotcha moments for the errant slip like mentioned earlier should not be the basis for penalties.
If I have three hundred patient contacts in a week, should I be cudgeled for one of twenty misses versus the wayward specialist and his fifteen out of thirty showing? It’s a matter of who is watching when and when the proverbial cameras are rolling.
I point out the above, of course, to illustrate the difficulty in making a system both fair in its penalties and near one-hundred percent hygiene compliant (probably more like ninety to ninety-five).
I attempted to cost out the price of a monitoring system–probably the only way to proctor adherence well. Unfortunately, I could not find more than a few links with figures.
To produce a sound analysis, we will need a precise apple to apple ROI comparison of monitoring technologies with transition coaches, diabetic educators, telephonic communication systems, and pharmacist time for medication reconciliation and post-discharge callbacks. Competing mandates and a lack of free capital creates an investment quagmire for hospitals. You pick.
But if CMS is reading, I have another option.
Assemble a moderately sized pod of hospitals, matched on demographics, payer, SES, bed size, etc., and keep them as geographically proximate as possible. If they compete, even better. Have them decide on a monitoring system they will purchase together at a discount (I hear vendors like big orders). If CMS has a little seed money sitting in a slush fund, still better. Alternatively, maybe even condition participation on a half-percent penalty give back from another program like the HRRP or VBP.
All the institutions must agree on the rules of the multi-year monitoring project, and each must publish their sum scores in a publicly accessible database (individuals would be held harmless for this endeavor). The catch? The bottom performers pay a penalty into a patient safety fund–one significant enough to make the bean counters take notice, but not enough to discourage continued participation.
However, there is another catch: CMS cannot touch the lucre. It funds worthwhile QI efforts of the mini-consortium, overseen by a self-appointed, representative board and approved by the Feds.
(Restrictions apply, of course, and the headline purchased by the victors in their local papers cannot read, “Hey losers, you owe us 5%. Also, before you give us the check, wash your hands. Oh yeah, prospective patients are forewarned.”)
Oversimplified? Yes. Crazy? No. But you get the picture.
All kidding aside, regardless of how you monitor handwashing compliance, if penalties translate to individual and hospital hurt, financial or otherwise, folks must buy in. The guts of any modern day solution will require technology and upfront costs. Anything less will lead front-line providers to push back and harbor more ill will against a regulatory system they increasingly see as suffocating and harsh (read: n=10 on a core measure). Occasional and mediocre monitoring just won’t do.



[…] version of this article originally appeared at The Hospital Leader, the official blog of the Society of Hospital Medicine. […]
[…] version of this article originally appeared at The Hospital Leader, the official blog of the Society of Hospital Medicine. […]
[…] chronicle of this essay originally seemed during The Hospital Leader, a central blog of a Society of Hospital Medicine. […]
Hi Brad,
I think that it is a very well written article by Bob Wachter on one of his favorite topics namely patient safety. I agree with your fools up blog about the penalties to providers for helping improve compliance. A carrot and stick approach could go a long way in motivating providers towards hand hygiene practices. One issue would be funding for monitoring this, health system with limited budgets might need alternate means of inancing projects like these in the interest of patient safety.
Rupesh.
[…] bit of a sting. Your stated preference. August 27, 2015 MedPage Today, originally appeared here on The Hospital Leader […]