Seen the State of Hospital Medicine report for 2018? I have, and there is erudition galore. Here is one that has me contemplating.
I was surprised to see the breakdown below. Not so long ago, I would say less than ten years, the scatter for adults was more balanced. By that I mean, the 99222 codes were more prevalent. To see seven out of ten submissions go high complexity over the last decade is an interesting change. Why?
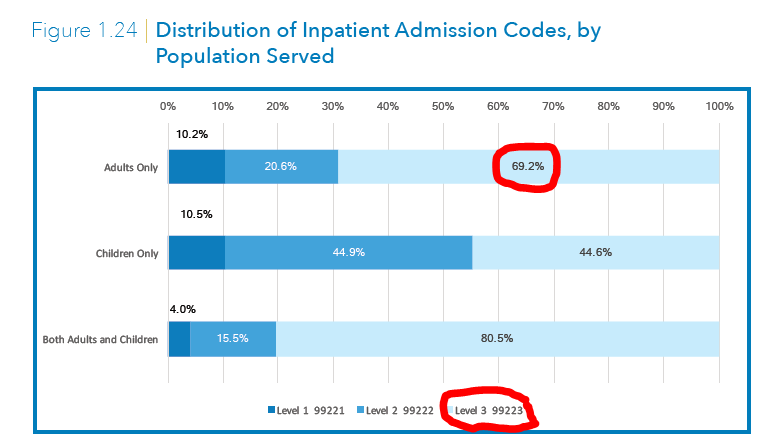
Well, if you accept the concept of “the normal” hospital patient, we should see perhaps a, 20% low, 50% intermediate, and 30% high complexity distribution. That is not the case. There is a name for what is happening, and it’s a big problem for payers. Its called code creep and invariably, in any reimbursement system, there is a tendency not to code to the individual in the bed, but to the documentation itself (for more dollars and to show “sicker” folks). EMRs have made this easier by allowing providers to include in their records elements they might have glossed over in the past. Additionally, EMRs have also allowed us to blow in note elements that boost the intensity of illness and to adhere to regs to boost CMI, again, for reasons mentioned above.
This is a survey, albeit a big one, and CMS can fact check how hospitalists code (we have a specialty designation as of 2016—we will know soon enough). if they want to put the kibosh on this, they can rebase payment or audit high profile systems. Word gets on the street fast. But even if they wished to build a better mousetrap, by paying by time lets say, docs will suddenly bill at the 26th minute (if the break to high complexity is 25). We always find a way–and it’s a cat and mouse game in perpetuity until it is not. CMS is talking big on this now and we at SHM are involved and want to provide guidance when and if the feds go full on E&M postal.
So what’s the answer?
That is a separate post, but global fees are one. But its hard to do and patient care attribution is hard to measure. Theory eats reality for breakfast.
Theories on the displaced and misplaced 99222 welcome.



The Medicare Administrative Contractors have already started auditing physician E&M coding of Medicare patients as part of their Targeted Probe and Educate program. Office, hospital, SNF will all be scrutinized, as will critical care. Doctors would be wise to look at their own code distribution within their billing systems and to check the public database at https://projects.propublica.org/treatment/
I teach residents a lot about billing and coding. I try to convince them over and over to make sure they give themselves credit for all their MDM. They too often model after other hospitalists and consultants whose HPI is limited to “no overnight events” and whose plan is “continue current plan.” I have NO idea what those folks are billing, but if they’re claiming credit for anything close to a 99222 (which clearly wouldn’t hold up in an audit), then those of us using our brains and our fingers should easily reach 70% high complexity in a day. Someone’s hemoglobin dropped and you had to do some MDM to catch that it was most likely because they were left on IVF overnight? Then document your through process, assume some risk (something we forget about as important in justifying complexity), and give yourself credit for a NEW, ACUTE diagnosis by including the relevant HPI elements.
Can you shed some lights on expected benchmark on these coding level and what point one should really get concerned? based on personal experience, in a small community hospital of <100 beds with few specialty back ups may not see a 99223 more than 20% of time.
We know patients are sicker with an increased chronic disease burden. Big shift of lower acuity patients to observation status (they have unique codes). ‘Blown in’ EHR data actually has very little impact on coding (unless as a provider you skip items like history while doing an H&P then take credit for the EHR data…?) because it is non-specific and does not have MDM value without additional comments (but does make notes unreadable and useless clinically).
Clinicians also becoming more familiar with actual E/M requirements and it is VERY easy to get to level 3, especially in the ER patient (coincidentally about 70% of our local admissions) with lots of testing already done for review. I do love the idea that this might incentive global payment, though the PB differential for 2 vs 3 initial visit in context of an entire hospital stay may not be significant enough to force meaningful change
Hi Brad,
I think there are multiple ways to interpret this data. While it has become relatively easier to meed the documentation requirements with the availability of EMR systems, it is likely that the skewed distribution is the result of increasing complexity of patients that we care for. An important consideration would be the data for Observation patients. Health systems could benefit from regular internal audits of their documentation and billing practices, to evaluate for any trends that would indicate code creep.
Rupesh.
Thanks for sharing.
Nearly all of my admissions are 99223’s. After all, it’s very easy to have a comprehensive history and physical (if you are documenting appropriately), and even “simple” chest pain admissions require a great deal of complexity – independent review of EKG, CXR, labs, ordering testing, summarizing old records). I can’t think of too many admissions that wouldn’t meet the 99223 threshold.
I agree with Jason. With the advancement in the healthcare, there is no more simple or easy admissions to the hospital. All the simple cases are not being admitted. So literally there is no value for 99221. And most of the admissions are complex, especially with dividing into Observation status and inpatient status, that dilutes the coding again. I cant think of too many admissions wouldn’t meet the 99223 threshold. An admission to the hospital should be either 99220 or 99223 or 99291. Nothing short of these codes.