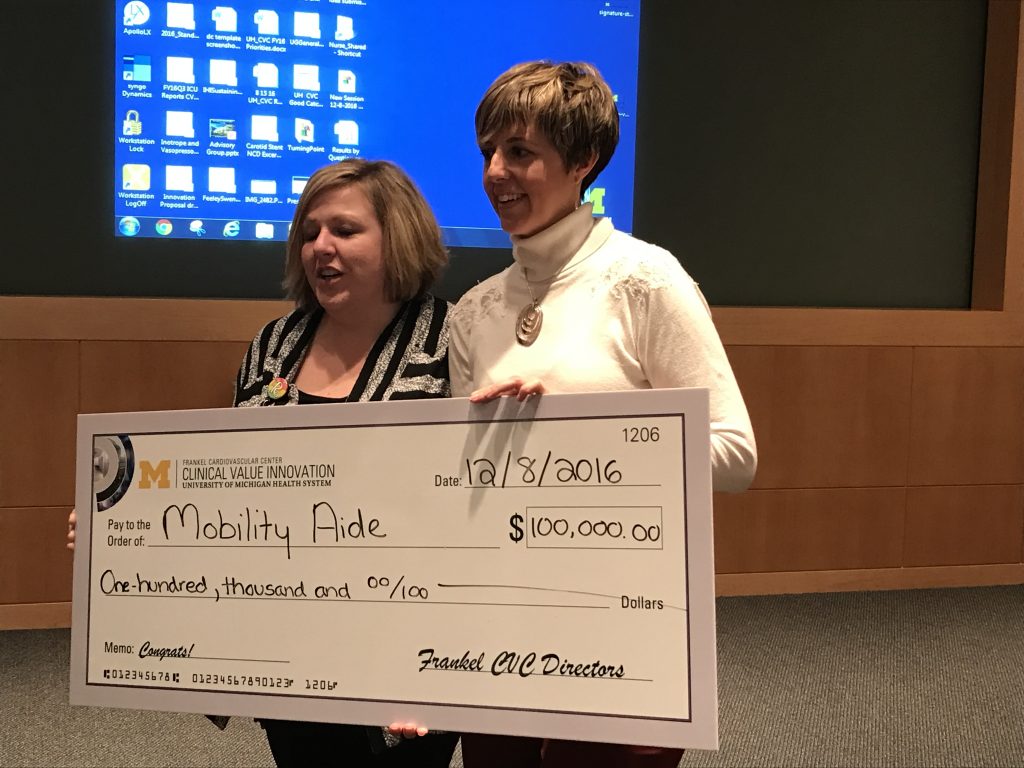
Earlier this month, I took a day trip to the University of Michigan Frankel Cardiovascular Center for their inaugural value challenge. Little did I know that when I arrived, I would be part of an all-star judging team that would be giving away $100,000 (a.k.a. real money) complete with a “big check”, a la Publisher’s Clearing Hou se, to the best idea to improve value! Given that I do not see patients on our cardiology service, I was starting to wonder if I was in over my head.
se, to the best idea to improve value! Given that I do not see patients on our cardiology service, I was starting to wonder if I was in over my head.
The good news is that value was defined quite broadly by different stakeholders; I was able to follow along, even though I wasn’t up to date with the latest in intra-aortic balloon pumps. We heard from 5 finalists. Interestingly, 3 of the ideas centered on specialized teams to improve care coordination for specific conditions such as atrial fibrillation, pulmonary embolism, or cardiogenic shock.
While all of them were quite interesting – and I am a sucker for any project that improves team communication – I had a nagging feeling that these would be a harder sell to improve value. I was not alone. My co-judges felt similarly that care coordination, in the end, may actually cost money – a viewpoint similar to one described by an editorial in the New England Journal of Medicine. However, that is not to say we should not advocate for care coordination. As the editorial states, “We should coordinate care not to save money but because coordinated care is better care.”
Interestingly, the people’s choice was a mobile app that would be a better way to define frailty and screen patients before surgery that were appropriate for “pre-hab”. While definitely cutting-edge, the challenge was generating return on investment in 1 year. That is a high bar for any app that has not yet been developed.
Not surprisingly, the winning project centered around the simplest idea—improving mobility for patients who were post-op cardiac surgery using a simple ‘walker’ that would enable all of a patient’s tubes, lines, and monitors to be connected to one platform instead of having multiple things to mobilize with. This idea originated from nursing and physical therapy, which also made it unique.
Sometimes, the best ideas to improve value are not only the simplest, but are the ones that originate from frontline staff. While the idea of crowdsourcing ways to improve value is not new – and has been previously described by the UCSF Caring Wisely Program as well as by Costs of Care in Academic Medicine – the excitement and enthusiasm for the event did not feel old at all. In fact, there was probably an even greater excitement that this work was being led by an interdisciplinary group of cardiologists and cardiac surgeons, including trainees. Of course, I was excited to see hospitalists involved as leaders of the event – namely Chris Petrilli and Lauren Heidemann.
So, as hospitalists, what can you do to get involved? Here are three easy things to do in the New Year:
- Submit an idea to improve value at the frontline to the annual Creating Value Challenge sponsored by Costs of Care. Any and all submissions are being accepted here before January 24th. Winners will get to present at the AAMC Integrating Quality meeting in Chicago in June. And new this year, institutions that have more than 5 submissions will be recognized by Leapfrog.
- Then, please join us for our next #JHMChat with University of Michigan hospitalist Chris Petrilli who will discuss his latest paper in the Journal of Hospital Medicine on “Things We Do for No Reason: Inherited Thrombophilia Testing.” (CME is available.)
- Attend Hospital Medicine 2017, where there will be a dedicated High Value Track for the first time! In this one case, whatever happens in Vegas should not stay in Vegas.
So no matter what you think of how 2016 went, it’s time to come together and agree that we still have much to do in 2017—after all, our “value” as hospitalists is definitely linked to creating value in care.
Happy Holidays!



Leave A Comment