I’ve been writing a lot about hospitalist satisfaction and career sustainability, but a just-released report from The Physicians Foundation shows just how widespread low physician morale and disenchantment with their profession really is. Every other year, The Physicians Foundation, a nonprofit group focused on supporting the work of physicians and improving healthcare quality, conducts a massive national physician survey with the help of Merritt Hawkins, a national physician search and consulting company.
The survey invitation was sent out by email to every physician in the country for whom the AMA has an email address on file; 17,236 of the roughly 630,000 physicians who received the survey invitation completed the 39-question survey. I hope a good number of them were hospitalists.
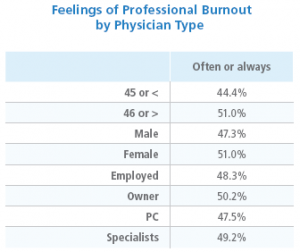
The report is chock full of interesting findings, and I encourage you to take a look. Among the highlights, the survey found that more than half (54%) of respondent physicians rated their morale as somewhat or very negative, and only 37% said they felt positive about the future of the medical profession. Just about half (49%) reported often or always experiencing feelings of burnout.
 Fully 80% of the physicians said they are at capacity or overextended, with no time to see additional patients. Only 14% of docs reported they have the time they need to provide the highest standards of care, and 72% said that external factors such as third-party authorizations and EHR design significantly detract from the quality of care they can provide. Here’s an amazing statistic: the respondents reported spending about 21% of their time on non-clinical paperwork; the authors calculated this to be equivalent to 168,000 physician FTEs not engaged in clinical activities!
Fully 80% of the physicians said they are at capacity or overextended, with no time to see additional patients. Only 14% of docs reported they have the time they need to provide the highest standards of care, and 72% said that external factors such as third-party authorizations and EHR design significantly detract from the quality of care they can provide. Here’s an amazing statistic: the respondents reported spending about 21% of their time on non-clinical paperwork; the authors calculated this to be equivalent to 168,000 physician FTEs not engaged in clinical activities!
Seventy-one percent of doctors rated “patient relationships” as the most satisfying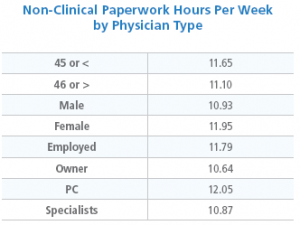 aspect of medical practice, while 58% said “regulatory/paperwork burdens” were the least satisfying aspect. On a related note, only 11% of respondents said that EHRs had improved patient interaction, while 60% said they have detracted from patient interaction. Sound familiar?
aspect of medical practice, while 58% said “regulatory/paperwork burdens” were the least satisfying aspect. On a related note, only 11% of respondents said that EHRs had improved patient interaction, while 60% said they have detracted from patient interaction. Sound familiar?
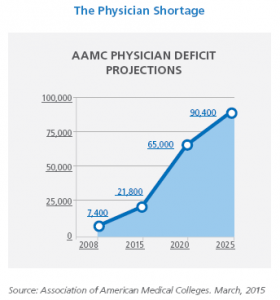
What are physicians doing about this? Well, 48% of them said they plan to cut back on hours, retire, take a non-clinical job, switch to “concierge” medicine or take other steps limiting patient access to their practice. That doesn’t bode well for physician access in the U.S. in coming years.
 Clearly issues of frustration and burnout among physicians are widespread and cross all age, gender, specialty and employment model lines. I urge you to keep that in mind the next time you have an exasperating interaction with your ED, cardiologist or orthopedist colleague.
Clearly issues of frustration and burnout among physicians are widespread and cross all age, gender, specialty and employment model lines. I urge you to keep that in mind the next time you have an exasperating interaction with your ED, cardiologist or orthopedist colleague.



Leave A Comment