One morning before rounds, my resident sheepishly admitted their disbelief that one of the patients we recently discharged had been readmitted. Our residents keep patients on their “epic list” and can easily see if they reappeared in the ED or the hospital. Certainly, this was a far cry from a study that suggested that if a patient is readmitted the hospital team did not even know!
Using the patient’s readmission as a safety teaching opportunity, we did our own mini M&M on what we could have done differently. Interestingly, we could not come up with anything! Even the PCP was shocked the patient was readmitted and thought what else could we have done. The patient, who suffered from complex chronic illnesses, felt well when they went home, but was readmitted a week alter with a different problem unrelated to their index admission. While this was just one patient, it’s not uncommon to care for readmitted patients and wonder what could be done differently.
In fact, a few years ago, I was on service and all of the new admissions were – you guessed it – readmitted. Many had been admitted to nearby area hospitals or to our hospital but were cared for by our team. Two were patients we had discharged. What were the reasons for the readmissions? Well, part of the reason included patient behavior – one woman had sever hypertension who readily admitted to lots of salt intake. Despite new medications as well as intensive counseling about her diet and avoiding low salt foods by a nutritionist as well as our team, she was readmitted after her blood pressure skyrocketed after she succumbed to her favorite friend chicken during the Sunday football game.
Another patient was discharged from another hospital with pancreatitis and despite counseling and referral to mental health services, he continued to drink over the week and came in for worsening of his pancreatitis. Another patient well known to the ER called EMS whenever she got depressed or lonely. After the fifth EMS trip to her house, she was brought to the ED who admitted her so that EMS was not called back to her house. Lastly, one of the patients was readmitted after my intern called him to do a post-discharge phone call. He decided to bring him back because he was feeling lightheaded and having GI bleeding, a known complication of the blood thinners that we started him on for his heart disease.
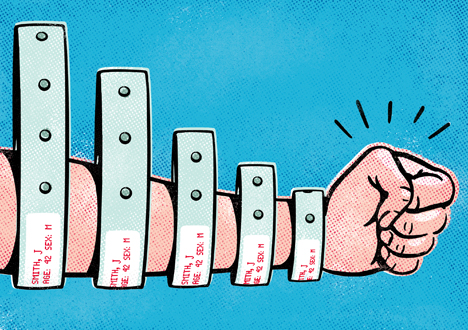
At the end of rounds, we wondered what could have been done differently. My residents, sensing my concern for the healthcare system, offered to run a ‘halfway house’ for our patients (conveniently at my house) to make sure our patients don’t get readmitted! Although my residents were joking (at least half joking), having hospital doctors and nurses ‘look’ for ways that readmission could be avoided assumes the problem lies in the hospital. In truth, the problem actually lies before they get to the hospital. All of these patients would benefit from much more social support and intense education and care for their chronic diseases, including mental health, which of course is woefully underfunded. While it is easy to pass the problem to a primary care physician who will maybe spend 20 minutes with the patient, the simple truth is that patients are largely responsible for their OWN care when they are not in the hospital.
So, how can we help these patients? The answer is not visible in their past medical history or history of present illness that has already been cut and paste from multiple discharge summaries to the next history and physical and so forth. The answer likely lies in their personal history of how they are able to manage their health struggles. Interestingly, the Association of American Medical Colleges recognizes this, and has recently launched a new approach to helping understand the reasons for frequently readmitted patients, by enlisting an unlikely workforce, medical students. The hotspotting guide from AAMC asks medical students to do their own mini-deep dive to understand why certain patients are readmitted using tips from Dr. Jeff Brenner of the Camden Coalition who was profiled in Atul Gawande’s landmark New Yorker article. In one step, the guide suggests that students should go to the patient’s home or place of residence “not to get a medical history but rather to better understand the patient’s personal circumstances, which will provide insights into this person’s struggles with getting care in an outpatient setting.” While the jury is still out on whether an army of able-bodied medical students can make a dent in readmission rates in teaching hospitals, the spirit of the initiative is on target. By understanding each patient’s unique story and values, we are more likely to better understand how to keep them out of the hospital.
So, how can hospitalists become hotspotters? Well, for starters, we can resist the abbreviated social history, or “no T/E/D,” which stands for no tobacco/etoh/drugs, to better understand the people and infrastructure that help patients to stay out of the hospital. We can also ask patients what THEY think would keep them out of the hospital. Lastly, we can interface with our hospital systems to identify these patients (we already know who they are) and brainstorm novel ways to try to keep them out of the hospital.
And before we completely dismiss the idea of hospitalists seeing patients in the outpatient sitting, it may be an idea worth testing…which is exactly what we are doing at our institution. With funding from the Centers for Medicare and Medicaid Innovation, the Comprehensive Care Program aims to provide some of the most frequently admitted patients with a physician who follows them both in the hospital as well as in the clinic. While this may sound like a return to the Marcus Welby of yesteryear, one unique difference and a large component to the program is the social workers, nurse practitioners, and administrative staff who form deep connections with patients both in and out of the hospital to better understand their social situation. Will we see a time when hospitalist teams follow their patients home? Stranger things have happened. Regardless of what the future may bring, we can all agree for any of our frequently hospitalized patients, there’s no place like home.


Leave A Comment