Two notable hospitalist studies out late last month–one from JAMA, and the other from JHM.
Association of the Work Schedules of Hospitalists with Patient Outcomes of Hospitalization
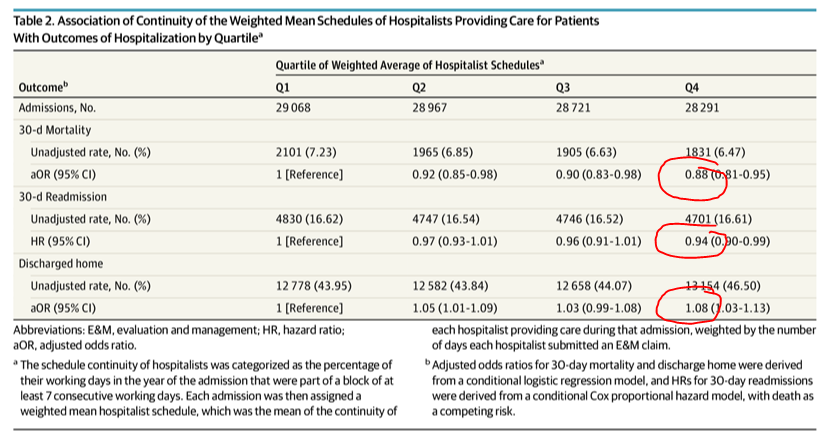
In this cohort study of 3 years of Medicare data from 229 hospitals in TX, covering 114K medical admissions of patients with a 3-day to 6-day LOS, patients receiving care from hospitalists whose schedules permitted continuity of care had significantly better outcomes, including lower 30-day mortality after discharge, lower readmissions, higher rates of discharge to the home, and $223 lower 30-day post-discharge costs.
The investigators used composites of hospitalist schedules per patient and broke out continuity into four quartiles. Q4 would be the greatest number of continuity days per patient and Q1 would be the least. You can see the outcomes of interest below in red.
The Bottom Line: Continuity matters. Surprisingly, there were fewer 7-day consecutive shift workers in this TX cohort than I would have guessed (less than half). Moreover, professional charges and HH use were higher in the Q4 group, whereas SNF use was lower (see table 3). The explanation may be state or culture-specific, or if analyzed deeper, perhaps continuity has attributes related to how PAC and specialist consulting are used by docs on service for longer (or fewer) consecutive days. I don’t know.
A Time Motion Study Evaluating the Impact of Geographic Cohorting of Hospitalists
This was a one site study out of Indiana. The investigators used both geotracking and observation to assess hospitalist direct and indirect patient time for 10K patient episodes.
In the 3K+ minutes of data obtained via in-person observations, geographic cohort hospitalists spent 56% of their day in computer interactions compared with 39% for nongeographic cohort hospitalists (P<0.005). Time spent multitasking in each group was similar (18% vs. 14%; P>0.05). Hospitalists in each group were frequently interrupted, but the highest rate, once every eight minutes in the afternoon, was seen in the geographic cohort group, which had a total of 139 interruptions versus 102 for the nongeographic cohort group.
The bottom line here: Geographic clustering has upsides, but it also comes with a cost. In exchange for more patient F2F time, hospitalist accessibility to ancillary staff increases. One could surmise, that grind will increase the intensity of working on clustered units and increase the risk of burnout. Also of note, the direct to indirect care ratio was 3:1, even-steven in both arms. Not a shocker as we know from past trials more time is spent on charting and EMR than direct contact. Marcus Welbys we are not.



I spoke with the author of the first study. unpiblished but per his review of the data, a 5 day block was not statistically different from the 7 day blocks re outcomes.
Regarding hospitalist schedules the most important “data point” should be physician lifestyle and burnout factor. Almost every hospitalist I speak to is happier if they work less days, see less patients and not miss their kids school/sports activities
This is a tricky situation, not only from a burnout perspective which could potentially be overcome by scheduling, but by movement of patients between units for level of care and retaining continuity. That certainly makes patient assignments unequal and less productive. I think attempting to maintain continuity of care by maintaining the same Hospitalist through the patient’s admission is important, as is ensuring the care coordinator and social worker understand the plan. Rounding with the nurse allows the nurse to reiterate the plan to patients and family members who might miss rounds. Just my two cents.
I agree with allowing the advanced practice providers to work at and bill at the top of their license. Following skills assessment, this should be the expectation and will be job satisfaction to hard working and extremely valuable APPs.
It was clearly shown about the Hospitalists, Geographic Clustering and schedules, The way you presented is great, Good information for all who visits the Hospitals. Nice Blog to read .