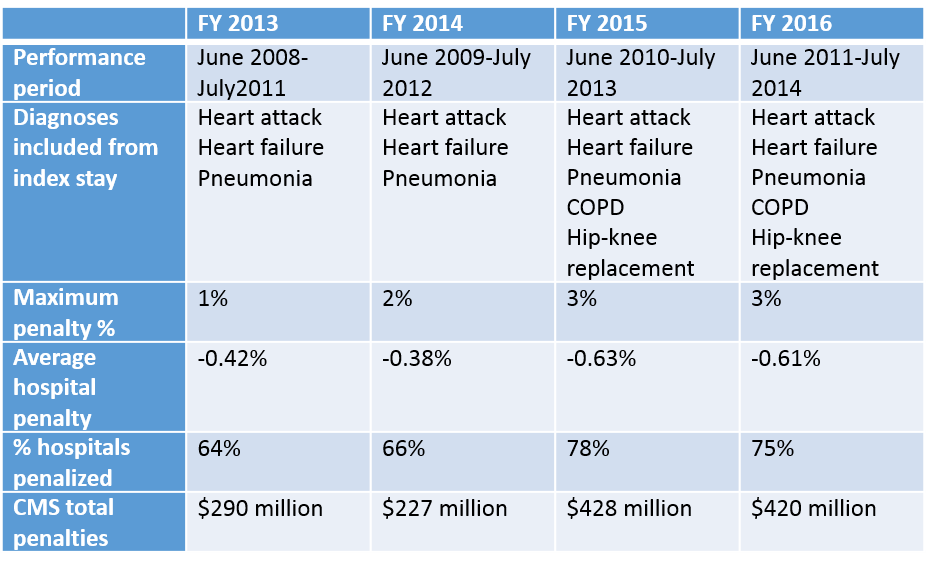
It’s that time of year again, when hospitals around the country are being notified of their 30-day readmission penalties from CMS. Now in the fourth year of the program, many hospitals have come to dread the announcement of how much they are being penalized each year.1 This year the readmission reduction program will decrease Medicare payments within a total of 2,592 U.S. hospitals, for a combined total of $420 million.2
 Unfortunately, safety-net hospitals were about 60% more likely than other hospitals to have been penalized in all 3 years of the program. In addition, hospitals with the lowest profit margins were 36% more likely to be penalized than those with higher margins.
Unfortunately, safety-net hospitals were about 60% more likely than other hospitals to have been penalized in all 3 years of the program. In addition, hospitals with the lowest profit margins were 36% more likely to be penalized than those with higher margins.
Despite criticisms of the program, there is no doubt that it has forced hospitals to pay keen attention to transitions of care and avoidable readmissions. And it does appear to be an effective strategy for CMS to achieve their goals; overall, there has been a decrease in 30-day readmission rates among Medicare recipients since the program began, in all types of hospitals. Compared to 2012, there were 100,000 fewer readmissions among Medicare beneficiaries in the U.S. in 2013. As such, there is no evidence that the program will be discontinued.3
What all this means for hospitalists?
For each of us working within the confines of the current program, there are few things we can all do to improve our understanding and performance within the program for our hospitals:
- If your hospital is one that incurred a penalty, know that most “eligible” hospitals also incurred a penalty.
- Look at how your hospital fared within your state and if you are above or below average in the amount.3
- Continue to focus on exemplary care transitions protocols, policies, and programs within your hospital system, as the penalties are unlikely to go away, and are very likely to expand over time.
- Support any advocacy efforts towards improving risk adjustment methodologies for readmissions, as all hospitals are likely to benefit from more accurate risk adjustments.
- 2. Half of Nations Hospitals Fail Again to Escape Medicare’s Readmission Penalties, Kaiser Health News



Leave A Comment