By Chris Moriates, MD
There is something oddly comforting about those morning labs: a ritual that I wrapped myself in during residency. Like swirling the milk into my cup of coffee, it is something that I do deliberately but only half-consciously each morning – make a list of my patients for the day, look over their vitals, and review their morning labs. I became a ninja at repleting potassium, hitting a “K=4.0” precisely, playing that game many play when filling their car with gas, trying to get the numbers to stick on a round amount (this potassium repletion more often than not was likely just as meaningless).
Now nearly everybody – including me – is agitating for us to lose this part of our morning routine. No longer are there always lab results magically waiting for me when I arrive at the hospital. (During my residency, did I ever stop to think about the reality behind that magic? The vampirical phlebotomist waking up my patient at 5AM with a needle and lab requisition that carried my name). The daily lab always gave me something to do and a checkbox to fill-in for each patient. It felt important. This will not be an easy habit for us all to break.
The SHM Choosing Wisely list challenges us to not “perform repetitive CBC and chemistry testing in the face of clinical and lab stability.”
Of course, that recommendation is difficult to disagree with but also elusive to implement. What exactly defines “clinical and lab stability”? Is stability something that oftentimes can only been appreciated in retrospect?
This is why I love being a hospitalist. Hospitalists did not just pay the recommendation lip service or brush it off as too vague. Many across the country – from Swedish Hospital to Vanderbilt to UCSF to numerous others –got to work on figuring out how to make this essence a reality.
Ok, But How?
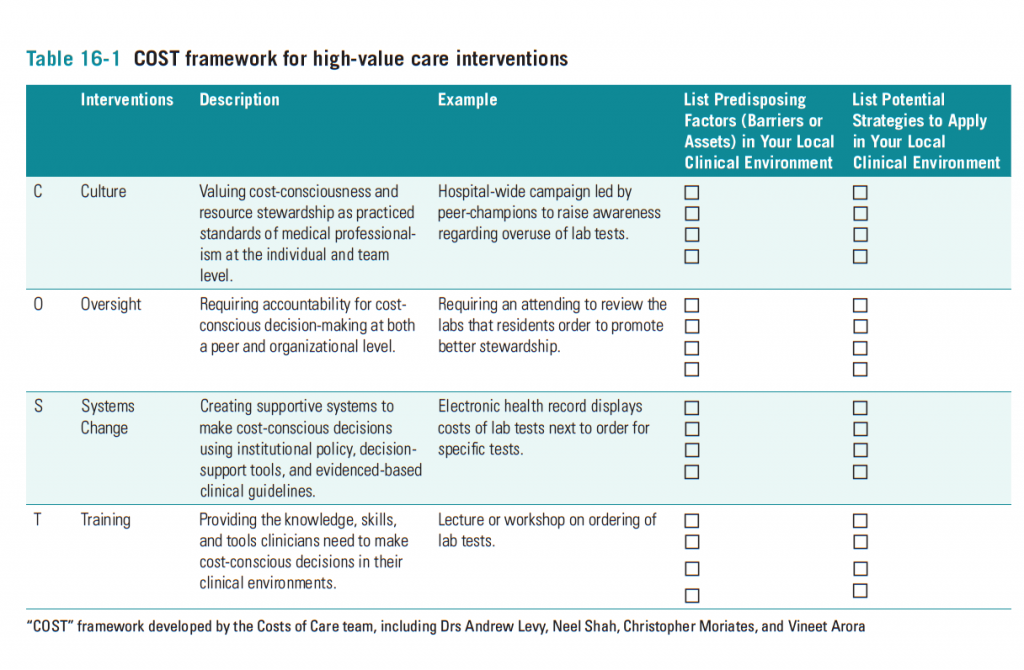
As we discuss in the last chapter of our book, Understanding Value-Based Healthcare, attacking a problem so deeply ingrained in habit and culture requires a dedicated, multipronged strategy that addresses culture, oversight, systems, and training (“COST”).
I have the privilege of working with a group of residents at UCSF who created a “Think Twice, Stick Once” project aimed at decreasing phlebotomy rates for hospitalized patients on the medicine service. There are a few things that I think were vital to this project’s success.
Here is how the 1st phase of the project targeted each of the “COST” areas:
Culture:
- Visible resident physician leaders
- Patient-centered focus by emphasizing number of “sticks” (rather than number of tests run by the lab, a metric that may not necessarily capture hearts and minds)
- Posters in the resident workrooms featuring the residency program director – a well respected and established physician role model
- A campaign with buttons and pens that feature the slogan, “Think twice, stick once”
Oversight:
- Team-based phlebotomy data abstracted from Epic was reported twice monthly to members of all 8 Internal Medicine teams, including data from peer teams for comparison (Figure 1)
![Figures and data from: Wheeler D, Marcus P, Nguyen J, Greenblatt R, Kahn T, Kwong A, Yee K, Valencia V, Moriates C. Think Twice, Stick Once: An Internal Medicine Housestaff Incentive Project to Reduce Phlebotomy [abstract]. Journal of Hospital Medicine. 2015; 10 (suppl 2). http://www.shmabstracts.com/abstract/think-twice-stick-once-an-internal-medicine-housestaff-incentive-project-to-reduce-phlebotomy/](https://blog.hospitalmedicine.org/wp-content/uploads/2015/10/Moriates_Chris_MouringLab_Image3-1024x1006.png)
Figures and data from: Wheeler D, Marcus P, Nguyen J, Greenblatt R, Kahn T, Kwong A, Yee K, Valencia V, Moriates C. Think Twice, Stick Once: An Internal Medicine Housestaff Incentive Project to Reduce Phlebotomy [abstract]. Journal of Hospital Medicine. 2015; 10 (suppl 2). http://www.shmabstracts.com/abstract/think-twice-stick-once-an-internal-medicine-housestaff-incentive-project-to-reduce-phlebotomy/
- The medical center’s “QI Incentive Program” adopted the project, providing housestaff with a financial incentive ($400) for meeting the stated performance goal – a small incentive, but one that helped elevate attention to the program
- The team has been working on changing the way that “add-on” orders for labs are handled by the lab workflow to ensure that these labs are reliably added-on to prior samples
Training:
- Phlebotomy reduction strategies introduced during monthly housestaff orientation sessions
- A “Facilitator’s Guide” for attending physicians with suggestions for discussing appropriate use of lab tests with trainees
- Discussions at monthly didactic sessions regarding best practices for lab ordering as well as a strong emphasis on the patient experience of phlebotomy
What specific strategies can we each use for decreasing lab use?
The first habit to break is to stop ordering labs as “daily” or “qAM,” but rather to order labs each day one at a time. I personally decide whether or not to order morning labs for the next day when I am writing my progress note for that patient, which lets me think about if any labs are needed and what they will be. We can also order non-urgent labs with the next scheduled lab draw, or add-on to existing samples. For example, if you want to get a TSH, you can almost always just order for it to be drawn with the next labs rather than as an additional stick. Alternatively, you can often add-on this order to an existing blood sample in the lab.
We also found that oftentimes interns were being contacted in the afternoon by the fellow of a consulting service, say ID or rheumatology, and asked to send a battery of serum tests. Usually in the interest of the intern’s workflow, these tests would just be ordered then and there, resulting in an additional lab draw. Many of these studies do not return quickly, and thus waiting until the next morning often suffices. Clarifying with consultants if labs are required urgently or if they can be drawn the next morning can be a helpful way to avoid the afternoon needlestick for our patients.
The ROUTINE morning lab is yet another a tradition in medicine that we must say goodbye to. While we hospitalists may somewhat miss it, many of our patients will happily bid the wake-up arm poke with a “Good Riddance.”
On a separate but related note, please join me (@ChrisMoriates) next Monday, October 12th at 9PM EST for the first #JHMChat, a twitter chat hosted by the Journal of Hospital Medicine (@JHospMedicine) on some of my recent Choosing Wisely: Things We Do for No Reason research. Click here to learn more about #JHMChat.



Leave A Comment