Most physicians recognize the JNC guideline for blood pressure management, or the ACCP thrombosis guideline for VTE. Most would agree we use a handful of accepted benchmarks to manage a limited number of conditions. For the rest, it’s the wild wild west.
Try to develop consensus around delirium management or treatment of alcohol withdrawal, and you will likely find yourself on the road to nowhere.
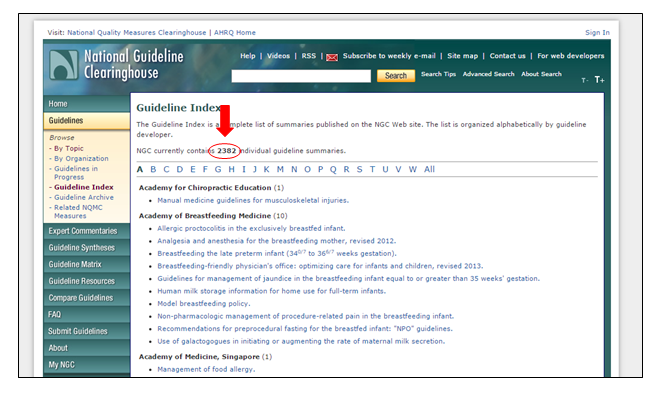
If you have never visited The National Guideline Clearinghouse, you should have a peek. Sometimes I find the site helpful for a management dilemma or patient with a rare presentation. However, for most, the compilation runs endlessly long and you will begin a convoluted journey if you crave a solution. The same road to nowhere.
As of this writing, the database has close to 2400 entries. Have fun with that:
In addition, given today’s emphasis on providing not just health care for our patients, but health, agencies and funders must afford concerned clinicians the opportunity to pursue topics usually banished to the bottom of the do list. If my years of experience have taught me anything, without question, toys and technology do half as much, for twice the price, relative to the unexciting stuff most take for granted. And you know what I mean by unexciting: care transitions, avoiding polypharmacy, patient activation, and utilizing available social supports to bridge patients back to the community.
You would not know it given our current funding priorities. I am certain if I listed twenty-five conditions and asked you to order them based on need, and then compared them to what those same conditions actually received, your list would be wide of the mark. By a lot.
Here’s what I clipped from the NIH. While subcategories may be hard to qualify and quantify, no doubt care transitions and the rest wont be perched at top:
This gets me to what I really want shine a spotlight on today: a new Journal of Hospital Medicine release entitled, A Patient-Centered Research Agenda for the Care of the Acutely Ill Older Patient.
With the opportunity to obtain new channels of funding and coalesce stakeholders who wish to speak out and provide input on how we should approach the unwieldy care of the elderly hospital patient—who make up a third to half of our census—a group of well-known and talented hospitalists responded with a major project.
They assembled a who’s who of organizations involved with geriatric care and used rigorous methods to cultivate a list of priority questions on which we should target future study. Again, with the shifting focus of health reform, groups like SHM will be at the center of how to rechannel what at times, seem like a sclerotic research enterprise. This document is exactly what we need. No one wants two thousand more guidelines to go missing.
The paper reads easy and the list of findings the group consolidated merits review. Take a look.
In addition, the principal investigator, Heidi Wald MD, MSPH, was also kind enough to answer some questions about the endeavor, in addition to commenting on the current state of how we deliver acute geriatric care. Below, you will find a briefly edited version of our conversation:
BF: Hi Heidi, and thanks for taking the time out to speak with me. What a job. How does your final agenda differ from the one you would have imagined? In other words, did the group’s iterative process change your perspective on what really matters?
Wald: I was surprised that there were few disease-specific questions such as strategies for anticoagulation in atrial fibrillation, or diagnosis of UTI in patients presenting to the hospital from nursing homes. The questions were primarily geared toward the geriatric conditions and delivery of care.
While the later prioritization steps refined the list of research topics, the nature of the list had already been shaped by the questions submitted by the survey respondents.
BF: When engaged in stakeholder gatherings, I am also surprised by the viewpoints that patients and caregivers relay. They can listen to a group of clinicians discuss “what matters” and think we come from another solar system. Did they surprise you in what they brought to the mix of concerns?
Wald: Absolutely, and that is the point of expanding the diversity of voices who have input to the research agenda development. Unless we bring patients and caregivers into the process, we cannot be sure we are addressing research to the areas of highest impact for the end users.
BF: A common refrain, “does funding drive research or does research drive funding,” embodies a difficulty you might have faced in assembling your list. As you point out in the paper, the topics chosen cut across specialties and lack specificity and pizzazz. You expended a lot of effort to hopefully open a door we often cant budge. What’s different this time? Why won’t this list of research priorities sit at the bottom of someone’s drawer?
Wald: (As an aside, pizzaz is in the eye of the beholder! Ten years ago, who would have thought that care transitions, readmissions,or catheter-associated urinary tract infections would become hot topics?)
PCORI, the Patient-centered Outcomes Research Institute, courtesy of the Affordable Care Act, has been been incredibly influential in shifting the focus of biomedical research from one driven entirely by researchers to one driven more and more by diverse stakeholders such as patients, caregivers, and clinicians in partnership with researchers. PCORI’s methodology report (one of our co authors David Meltzer is a member of the methodology committee that wrote that report) set new standards for this approach to research. PCORI used a similar approach to drive its overarching research prioritization process. PCORIs work has yielded research that is similarly focused to our agenda. For instance, you will notice that falls did not make it onto our list. It was up there but was removed in the last round of balloting as PCORI has already funded this priority. Further this list is very aligned with national patient safety goals such as the reduction of Hospital-Acquired Conditions, and focus on care transitions. Finally, some funders were at the table in our prioritization process. Thus, we believe this list will be readily adopted by our stakeholders.
BF: You have been in the geriatrics learning game for some time. Do you think hospitalists have progressed any faster in this domain relative to other specialties in frequent contact with elderly folks? We often tout our “unique” vantage point, but I am not so sure. Do you feel hospitalists have a leg up. Are we a bit more advanced in our understanding of the geriatric patient?
Wald: Ten years ago I published an article in JHM that showed very little innovation in geriatric care models in hospital medicine groups. If we repeated that work now (it is on my to do list!), I think we would find a very different landscape. For instance, at the University of Colorado, we have created an environment where we have sensitized our Hospitalists and our trainees to geriatric care issues primarily through an hosptialist-led Acute Care for Elders Unit (also published in JHM). To the extent that our national patient safety goals are influenced by CMS’s interest in the older population, Hospitalists and hospitals are incentivized to address these issues.
However, I don’t think we can generalize to the field of Hospital medicine and declare victory. We still hear the the question “Why are older patients different from younger patients?” And we still face systems barriers to providing the highest quality of care to this vulnerable population. Given the complexity of patient care, the fast paced environment in which we work, and gaps in training in geriatric care, it is all too easy to skip a cognitive and functional assessment or pass on a goals of care discussion. Dementia, delirium, and depression are missed; readmission rates are too high. There is plenty of work to be done.
Our group is very proud to be part of the Society of Hospital Medicine whose leadership supported this important project and has been very deliberate about incorporating geriatric care initiatives into its programming. This leadership will continue to have an important downstream effect for the field.
BF: Is there anything else you would like to add Heidi? Any pearls of wisdom you took away from this worthy endeavor?
Wald: As a researcher, I was impressed by the power of the stakeholder engagement process we employed. This method was grounded in qualitative research methodology which provided us with a valid and transparent process by which to create a very different type of research agenda. I was also overwhelmed by the volume of responses to our survey and the commitment and professionalism of all of our stakeholder organizations. I hope to see other groups adopt this powerful approach.
 Dr. Heidi Wald is an Associate Professor of Medicine in the Division of Health Care Policy Research at the University of Colorado School of Medicine where she serves as Vice Chair for Quality in the Department of Medicine.
Dr. Heidi Wald is an Associate Professor of Medicine in the Division of Health Care Policy Research at the University of Colorado School of Medicine where she serves as Vice Chair for Quality in the Department of Medicine.
Dr. Wald has a longstanding interest in patient safety and quality of care for the geriatric patient with a focus on the hospital setting. She led the Society of Hospital Medicine’s Acute Care of Older Patients Priority Setting Partnership. She has published in the areas prevention of hospital acquired conditions, models of acute care of older patients, infection prevention, sentinel event reporting, and root cause analysis.
At the University of Colorado Hospital (UCH), in addition to running patient safety and quality improvement program for the Department of Medicine, Dr. Wald serves as the co-director of the Acute Care for Elders Service, and leads the Multidisciplinary CAUTI Prevention Workgroup. In 2012, she received the President’s Award for Leadership and in 2014 she received the Clinical Effectiveness and Patient Safety Award, both from the UCH Medical Staff.




Leave A Comment