That was the old cardiology joke from a decade ago when job supply exceeded demand. The field seemed to get its groove back—through both supplier-induced and demand factors—but do not hold your breath. Workforce needs have only begun to get critical reappraisal and I would not rule out restaurant service for any specialty as health reform shakes out our sector.
Along those lines, as medicine becomes a team sport, ratios of doctors to nurses, PA’s, NP’s, therapists, and pharmacists all will undergo scrutiny. And as of 2014, I thought I had a handle on where things stood. As to pharmacists at least, I read the wrong playbook. I had no idea:
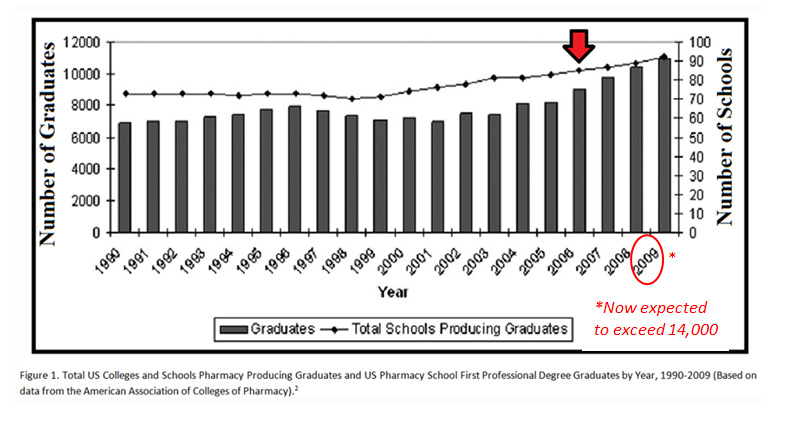
Now, the profession is on the verge of a crisis: The number of pharmacy jobs has dried up but the number of pharmacy students keeps growing. It’s difficult to find a cushy, full-time job and metropolitan job markets are saturated. PharmD candidates are graduating with hundreds of thousands of dollars of debt, and each year, there are more and more of them in a six-year-long pipeline. When Pak graduates in 2016 with a PharmD degree, he’ll have up to $150,000 in loans.
My estimate [is] 20 percent unemployment of new grads by 2018,” Daniel Brown, a pharmacy professor at Palm Beach Atlantic University, told the Pittsburgh Post-Gazette in 2013. “The job market is [stagnant], but we’re still pumping out graduates every year.”
Like veterinary school, false promises, proliferation of for profit institutions, and ambitious workforce projections have produced a mess. A major mess.
Given our close relationship with hospital-based pharmacists, we will find their current state of affairs relevant. The article notes pending legislation to expand the responsibility of pharmacists to fill care gaps in our system (with more bills to come).
Where appropriate, and I believe we need to expand roles—pharmacists can deliver services and education where the system has deficits. However, the profession has such a surplus; with schools desperate to unlock jobs and worthy salaries; and with a bloated healthcare system in need of contraction—not expansion , I envision an aggressive, internal push to move PharmD’s into myriad roles heretofore not seen, aka, “mission creep.”
In no way do I besmirch pharmacists and the work they do. Truth be told, when I work with them on the wards I find upside only. Rather, unsavory forces at the top need to act, and the action may translate to regulation for job repurposing, and yes, new billing codes. Think USDA and cheese. When you have a resource overage the market can sometimes act in funny ways.
In addition, the excess production of pharmacists exemplifies another flaw in the US health system. With a desynchronized workforce and a siloed education system sending and receiving bad signals, we produce market distortions. These distortions make a system fix more difficult and adds to the already herculean task of undoing decade’s worth of mischief.


Leave A Comment