Firstly, thank you David for taking the time to answer questions for the blog. You got my attention when you expressed, “the greatest excitement you have ever had in your career,” for your current CMS Innovation Center endeavor. Given your list of accomplishments, that is a tall order.
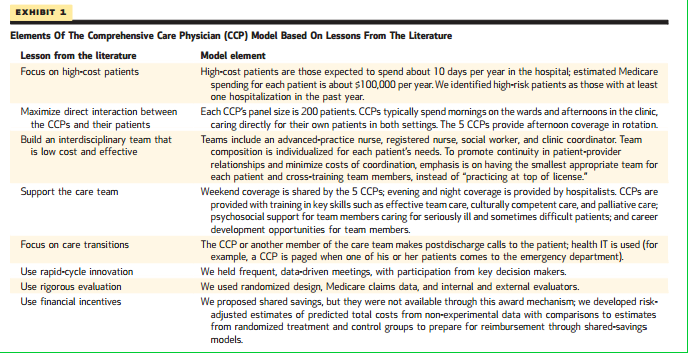
Secondly, I want readers to take note of David’s latest paper in Health Affairs describing his project, Redesigning Care For Patients At Increased Hospitalization Risk: The Comprehensive Care Physician Model, as well as his presentation at the accompanying publication briefing.
1. Let me say, if your paper delivers on its promise, we will see a real shake up in the way we deliver care to chronically ill, hospital prone patients. Based on the oversized attention you received at the Q&A following the briefing, others felt similarly. Can you review your project and give us the nidus behind developing the intervention?
The basic idea behind the comprehensive care physician (CCP) model is that patients at high risk of hospitalization may benefit from having the same doctor care from them in clinic and the hospital. To make this possible our model proposes that a set of doctors focus their practices on a small number of patients at high risk of hospitalization so that they can always have enough of their own patients in the hospital to justify their presence there. We think that the model combines the advantages of hospitalists in terms of inpatient expertise and regular presence and the advantages of primary care doctors in terms of continuity in the doctor patient relationship.
2. You noted in the briefing, RVUs and billing more than covered the cost of physician care. What a welcome surprise. However, the ancillary team and community resources depended on revenue support from the grant. A stream of money you will not have when the project expires. How do you envision continuing the work, and spreading the gospel to other sites, if the model has positive effects?
This is a key question. The most obvious solution would be to implement this in the context of a risk contracts for predefined populations, so savings would accrue to the hospital and support the costs of the program. Some institutions already have such arrangements on large scale but many do not. In the absence of that, a fee for service arrangement plus modest care coordination fees could be a reasonable alternative. We will also be seeking grant and philanthropic support to build on this work. One nice thing about our model is that it is not expensive to implement.
3. I noted a few of your comments, “division of labor has gone too far,” and “the hospital medicine model may benefit doctors more than patients,” as a foreboding look into the future. As one of the earlier investigators (and proponents) of hospitalist care, the position you stake out will strike some as inconsistent. Rightfully though, as you articulate, the evidence seems to have fallen short of expectations. If we go back to the future, and docs move in and out of the hospital to deliver services, where do you see hospitalists fitting in to the acute care model?
I have no fear at all for the future of the hospitalist movement. Hospitalists meet an essential need because primary car doctors and specialists are not well situated to provide hospital care for a large fraction of patients. Over time, expect the benefits of hospital medicine practice will grow as the field generates increasing levels of specializes expertise. The CCPs, which I have also sometimes called Primary Care Hospitalists, should be thought of as a complement to traditional hospitalists and a type of hospitalist, rather than as a rejection of the model.
4. On its face, this model really has appeal for practitioners: a great support team, a limited panel of 200 patients, and at least in your shop, highly satisfied docs and PGYs pining for similar positions. Do you think the potential for higher doc satisfaction embeds itself within this arrangement? After listening to your talk, I kept thinking, where do I sign up?
There are almost too many to convey. One is that a lot of patients will benefits from home care, so we now have a ccp who does hospital care in the morning and home visits in the afternoon. Another is that there is long learning curve in any care model and we are still learning how to improve care each day.
Thanks so much for sharing with us David. We anxiously await the findings from your trial.
Key components of the program:



Leave A Comment