by Dr. Douglas Mitchell MD, MBA
On January 10, 2014 the state of Maryland announced a new approach to hospital payments that would radically alter how healthcare is delivered in the state. Hospitals would no longer be incentivized to generate more volume but would instead be rewarded for keeping people out the hospital. Uwe Reinhardt, a health care economist at Princeton University said “This is without any question the boldest proposal in the United States in the last half century to grab the problem of cost growth by the horns.” Understanding healthcare reform efforts in Maryland requires a little bit of wonkiness but components of the Maryland plan will likely become part of national healthcare reform efforts. Like all change there are opportunities for people to excel in the new system, and in order to excel hospitalists need to adapt intelligently to the new environment.
A Little History for Context:
In 1971 the Maryland state legislature enacted legislation allowing a regulatory board (Health Services Cost Review Commission or HSCRC) to set reimbursement for inpatient hospitals. All private insurers were required to pay these rates. In 1977 the Center for Medicare and Medicaid Services (CMS) granted Maryland a waiver and allowed Medicare and Medicaid to pay Maryland hospitals the rates set by the HSCRC. Thus the Maryland All Payer system was born. The cost of uncompensated care was shared equitably across all payers. The system is unique in the United States as no other states have what is essentially a European single payer health plan.
In order to maintain the waiver, the increase in Medicare costs in Maryland inpatient care could not exceed the national increase in Medicare inpatient care. The All Payer system was effective at keeping the rate of increase below national rates for thirty-five years, however in 2012 Maryland failed the “Waiver Test,” and the system was unfortunately instrumental producing one of the highest rates of hospital readmission rates in the country (49th out of 51 states and the District of Columbia).
January 10, 2014:
Given the risk of losing the waiver, Maryland reformed its hospital payment system and in January 2014 CMS and the state of Maryland jointly announced the new program. There are two phases to this program. The first phase occurs over 5 years and is primarily hospital focused. To maintain the new waiver Maryland hospitals must meet the following five targets at the end of the first period (January 2014 to December 2018):
1. Limit the rise of per capita hospital costs to less than annual growth rate of the state GDP.
2. Save $330 million in Medicare spending.
3. Insure growth in Maryland Medicare spending does not exceed the growth in national Medicare spending.
4. Bring Maryland’s hospital readmission rate to the national average in five years.
5. Reduce hospital acquired infections and complications by 30% in five years.
To accomplish these goals the HSCRC is aggressively shifting its payment strategy from volume based to value based metrics. Hospitals receive a global budget based on historical volumes. The global budget can be adjusted based on changes in market share but generally hospitals receive the same revenue regardless of the volume of services provided. The HSCRC has also placed significant revenues at risk tied to performance in preventing readmissions, improving patient experience, decreasing hospital acquired conditions, improving mortality rates, and achieving patient safety initiatives. In 2017 Maryland hospitals will be eligible for a performance based 2% reward or 7% penalty based on these quality metrics.
What does this mean for hospitalists in the state?
First, and most dramatically, private practice hospitalists are being encouraged, coerced, and forced out of the hospital or into incentive based contractual arrangements. Under the new payment system Maryland hospitals cannot allow private hospitalists to practice with misaligned incentives when alternatives such as employed hospitalists or contracted hospitalists are readily available. This has occurred in five of the fifteen hospitals where our company provides services. And it has occurred in some instances despite significant political blow back from the medical staff.
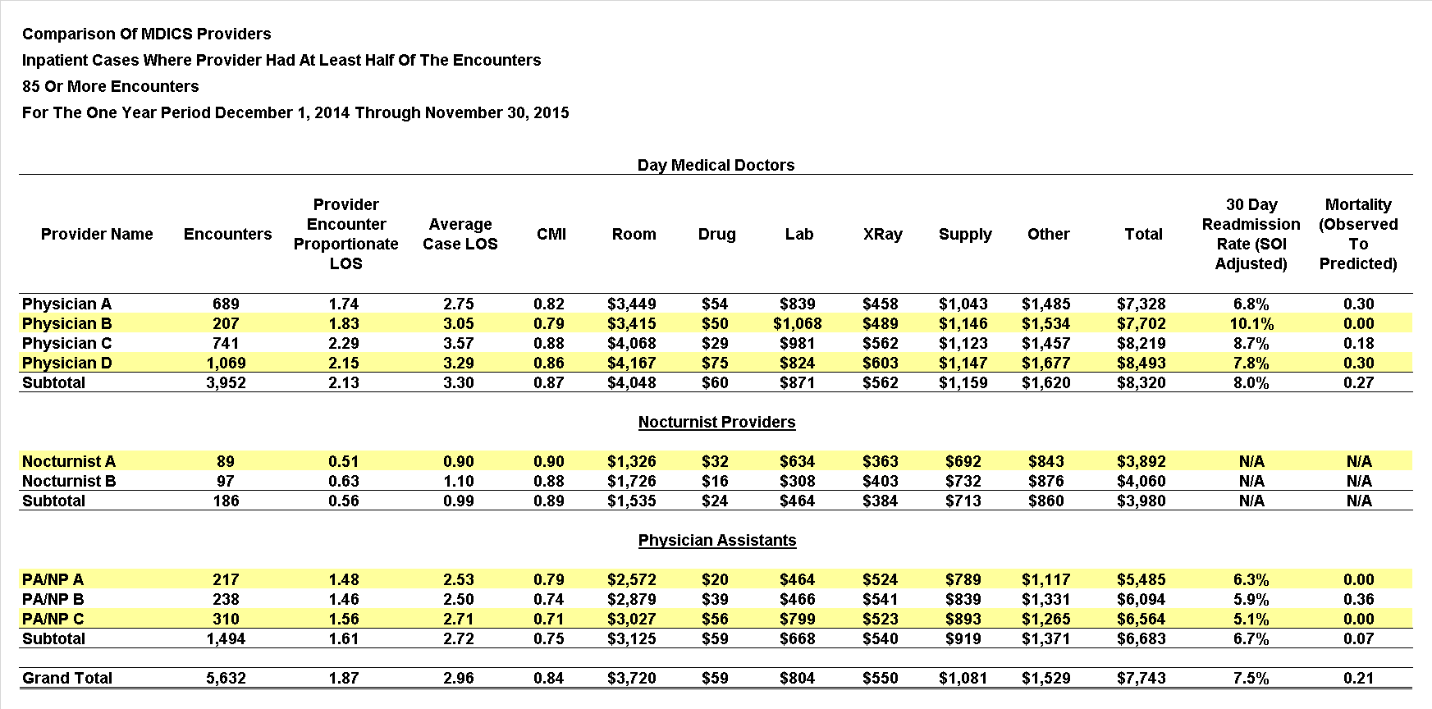
Second, hospitalist programs, whether hospital employed or contracted, are cost centers and not profit centers. As a cost center we justify our existence by demonstrating our value. In the new Maryland environment employed and contacted hospitalists are under more pressure to show value and are being monitored more closely so this value can be demonstrated. An example report that our group uses is shown here (click the table to view in a new window).
To better align group and individual quality goals a higher percentage of individual compensation is being tied to quality metrics. The number of performance measures being followed are increasing and these measures are becoming more granular. And most importantly, there is a move to disaggregate the group data and then tie performance to individual hospitalists (as demonstrated in the table above). In this pressured environment that ties significant revenues to achieving performance metrics not only will we see more quality based incentive pay but we will also see poorly performing hospitalists removed from employment and replaced with better performing hospitalists.
The last trend occurring with hospitalists in Maryland is that groups are being asked to provide care outside of the usual roles filled by hospitalists. Our group has been asked to provide pain management nurse practitioners (to help with the pain component of the HCAHPS scores), employ palliative care providers (to help with mortality measures), and staff discharge clinics (to help with readmissions). We are also forming collaboratives with non-hospitalist groups because many of the quality measures cannot be effected without a coordinated effort between several groups of providers. The elderly nursing home resident is always going to be admitted at 11:00 p.m. unless the geriatricians in the nursing home, the hospitalists, and the emergency room providers work closely to insure safe and quality care back at the nursing facility.
The states are our laboratory of democracy and in this case Maryland is a laboratory of healthcare reform. By radically changing payment incentives hospitals are being forced to change the way care is delivered to patients. And the first year results are promising, showing significant progress in attaining the goals. There is a lot of opportunity for hospitalists who understand and embrace the rules of the new environment. As always, the “B” word – Burnout – is a risk for hospitalists in the changing workplace. Hospitals though are desperate for people who can lead the change and hospitalists are uniquely positioned to provide this leadership. Successful leadership will require a commitment to more transparency and accountability for individual performance, a willingness to align even more closely with hospital goals, and an openness to work outside of the bounds of the normal inpatient internal medicine hospitalist care. It is a great opportunity for those of us willing to adapt to the change.



Great perspective and a very good read at that.