Costs in health care tend to concentrate in the domains of the few (think 80/20 rule). As it goes for chronically ill community dwellers, the same applies to frequent flyers in the ER. You may have heard of the term super-utilizers.
Those individuals present week after week with innumerable complaints, sometimes pedestrian, sometimes critical–always finding themselves back on the ward for weeks at a time. As expected, they have weak community support and comorbidities in need of TLC, often requiring services not available in their neighborhoods (mental health and substance abuse counseling come to mind). The local house of worship, community center, or corner bar have limits, and they only offer so much spiritual renewal or sustenance. We all struggle to find a balance for these folks. We see them a lot. And thus, the ER becomes their second home.
But do their frequent trips to the ER lead to more admissions and resource use?
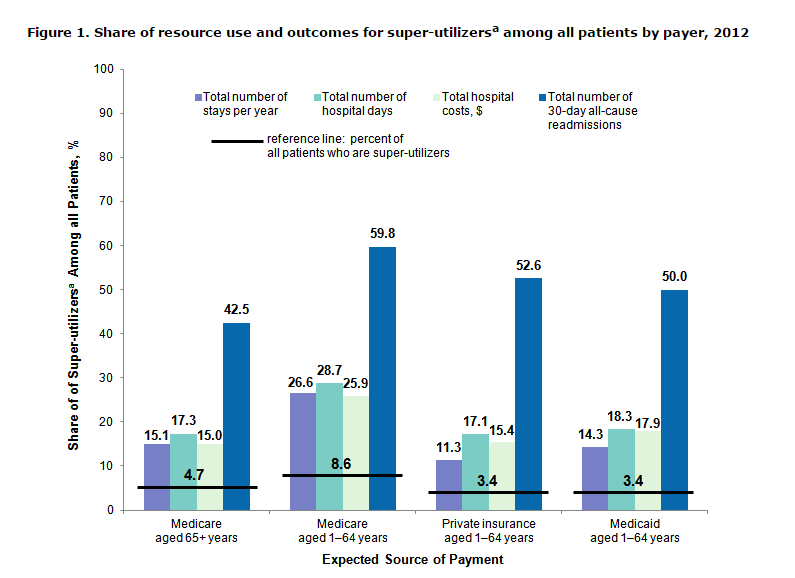
I have written about HCUP data in the past (another reason we can’t lose AHRQ funding). In a recent statistical brief, AHRQ looked at super-utilizers, defined as Medicare or Medicaid patients with four or more hospital admissions or privately insured patients with three or more hospital admissions in 2012. As a percent of all beneficiaries, they calculated their total stays per year, hospital days, hospital costs, and, in particular, readmission trips.
Have a look at the graph below. Soak in the black horizontal bands and vertical blue bars. About 5-10% of super-utilizers comprise 50% of readmissions.
Think about that. Three percent of Medicaid beneficiaries constitute fifty percent of readmits. Talk about signal to noise. As expected, mental health and substance use disorders were high in the top ten list of DRGs within the Medicaid (and privately insured) categories.
Me thinks teach backs and medication reconciliation won’t cut it alone. Problems at the non-Medicare level, we all know, require a lot of stamina to solve. Those recipients will consume energy in amounts our institutions, at least now, cannot deliver. Even with maximum effort, applying all the tools BOOST and Project Red have to offer–absent counselors, therapists, inpatient rehab programs, and safe shelters–our efforts will be for naught.
You will note some interesting, in-depth data within the brief and the tables will give you some grist to chew on when you consider the interventions best suited for payer and patient. One size does not fit all, and you must avoid confusing Medicare and Medicaid experience: they are of different realms.
Plus, here is an excellent JHM commentary on why super-utilizers require a more individualized, unique approach. The points made by the authors shed further light on why we need to consider the needs of these patients separately.



I sincerely appreciate the respectful and kind way this post was written. Because of that I am able to understand questions I had, much more clearly now. Thank you and know I will pass this on to others, who will enjoy it as well.
Hot spotters…As in the Camden NJ program where 1% of the 100,000 people who used the city’s 3 hospitals accounted for 30% of the city’s medical costs. That translates into just 1000 people…the super-utilizers.
Those of us in the hospital business have known about the ‘frequent flyers’ for years but with the move from volume to value have the costs associated with these patients become an issue.
The value of a robust care mgmt. program dedicated to these patients will have to be demonstrated. In collaboration with payers, the data can be used to identify patients who will best benefit from patient-specific care mgt strategy.
[…] “super-utilizers,” folks who consume a disproportionate amount of health care, and what this means for the rest of us “normal” […]
[…] Flansbaum talks about super-utilizers and how they impact health care delivery for the rest of […]
[…] Flansbaum talks about super-utilizers and how they impact health care delivery for the rest of […]
I think the point here is well made. Just as we are seeing development of targeted therapies for many conditions, frequent flyers/ super utilizers requiem targeted care coordination using multi-disciplinary teams involving inpatient and outpatient services and also community resources. This might help reduce the resource utilization by these patients.
Thanks.
[…] “super-utilizers,” folks who consume a disproportionate amount of health care, and what this means for the rest of us “normal” […]