As a personal advocate for value-based care, I was lucky enough to do my Hospital Medicine Fellowship at an institution that placed a strong emphasis on improving and optimizing value for its patients. As a (mildly naïve) first-year fellow, I recall being impressed by an atmosphere and culture that appeared to embrace the “less-can-be-more” movement. Yet as time went on, I found that while many wanted to achieve that goal, the pathway to getting there was not as straight and narrow as I’d imagined or perceived it to be. My friend and mentor, Vineet Arora, MD recounted to me how even though we all want to do the right thing, the process can be challenging. She recalls their story here on how difficult it was to just remove ONE lab from their order set:
“Several years ago, an enterprising resident came to me and asked, ‘Why do we order CKMB for acute coronary syndromes when it is not necessary?’ My quick answer? ‘Probably because we have always done it that way.’ He set out to do a value improvement project through our local Choosing Wisely challenge on improving lab ordering with a focus on CKMB. He used 3 techniques to highlight his argument: (1) Evidence: trials showed that CKMB was not a helpful marker and Troponin was more useful; (2) Peer pressure: several other prominent teaching hospitals had already removed CKMB without adverse consequence, and (3) Dispelling myths: specifically that CKMB was better marker of heart damage for those with renal disease.
While he had the support of cardiology faculty champions in advocating for removal of CKMB, it was not enough. In reviewing ordering of CKMB, we made no dent. When we asked the residents why not, it turned out that even though we had the support of cardiology champions, there were some influential faculty that were concerned about this switch–concerned enough that the residents were wary of removing CKMB from their admission orders. That got us wondering… was it just us, or were there other hospitals that were not ready to make this leap? What characteristics could predict if a hospital would be willing to adopt a less-is-more approach to cardiac biomarker ordering?
Fortunately, through a partnership with Vizient via University of Chicago, we had data from 83 teaching hospitals and millions of encounters that could answer this question…”
While the University of Chicago remains a leader in implementing and evaluating value-based care, even they must overcome institutional, cultural and psychological barriers to provide such care. And yes, they were able to overcome these barriers and implemented troponin-only testing for ACS.
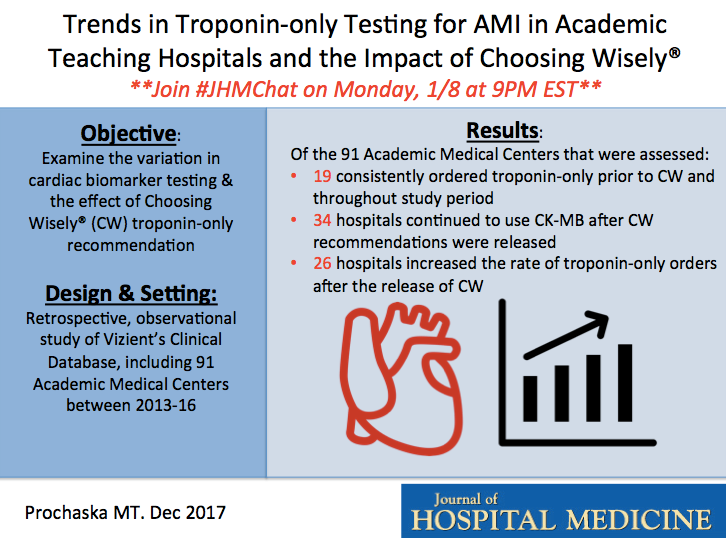
Given the recent 5 year anniversary of the advent of the Choosing Wisely campaign, we decided to highlight their article (“Trends in Troponin-only Testing for AMI in Academic Teaching Hospitals and the Impact of Choosing Wisely”) and discuss the effects of Choosing Wisely on ordering practices in this month’s #JHMChat on Monday, January 8 at 9 p.m. ET.
Not familiar with #JHMChat? Since October 2015, JHM has reviewed and discussed more than a dozen articles with many focusing on improving the value and quality of care we provide to hospitalized patients. Medical students, residents and practicing hospitalists are encouraged to join, as we discuss a broad array of topics that affect the care of the hospitalized patient. It’s a great opportunity to meet others, learn and even earn free CME.
Join me (@WrayCharles), guest author Micah Prochaska, MD, MS (@micah_prochaska), and ABIM Foundation Chief Operating Officer Daniel Wolfson (@WolfsonD) on Monday, January 8 at 9 p.m. ET, when we will discuss “Trends in Troponin-only Testing for AMI in Academic Teaching Hospitals and the Impact of Choosing Wisely”.
To participate, just type “#JHMChat” in the search box on the top right corner of your Twitter home page, click on the “latest” tab at the top left of the page and join the conversation. Don’t forget to tag each of your tweets with the hashtag #JHMChat. We look forward to having you join us!


Leave A Comment