Everywhere I go these days, one of the top questions on the minds of hospital leaders and hospitalists alike is, “How can we improve hospitalist patient satisfaction scores?” It’s a dilemma. There are people who know way more about this subject than me, but I’m not aware of anyone who has really cracked the nut. In nearly every hospital I’ve visited over the last few years, the hospitalists are struggling to improve “their” patient satisfaction scores, usually with limited success.
A big part of the problem is that it turns out these people are asking the wrong question. And as a result, hospitalist groups are all too often being faced with a burden they were never intended by public policy to bear.
The place to start is with a realization that CMS conceived HCAHPS specifically to measure hospital-level performance. Regulators never intended HCAHPS to be used to evaluate the performance of individual doctors, nurses, or other hospital staff, or to attribute scores to any individual physician (or physician group). In fact, CMS officials have made it clear that evaluating individual providers or linking provider or group financial incentives to performance on the HCAHPS responses of patients under their care is “contrary to the survey’s design and policy aim; HCAHPS is not suitable for evaluating or incentivizing individuals or groups within a hospital.”
HCAHPS is not measuring you on your patient experience performance, contrary to what many of you are being told by hospital and health system leaders. CMS is measuring the hospital’s overall performance with respect to patient experience, and your contribution as a hospitalist to your patients’ perception of their overall hospital experience, including their experience of physician communication, is only one of many factors that interact in complex and little-understood ways to influence survey scores.
What Do We Know About Hospitalists and HCAHPS Scores?
Many, including me, assume based on anecdotal experience that HCAHPS scores – including scores in the physician communication domain – tend to be lower for patients attended by hospitalists than for many others in the hospital. Unfortunately, CMS’ HCAHPS vendors don’t code “hospitalist” as a separate specialty, so I’m not aware of any published data that supports or refutes this common assumption.
But a June 2017 article in the Journal of Patient Experience assessed a variety of physician attributes and their relationship with patient satisfaction scores (both the CMS HCAHPS questions and some additional Press Ganey-specific questions). After analyzing 51,896 surveys, the authors found that males received top box scores significantly more often than females in the Press Ganey (not HCAHPS) questions related to being well-informed and provider skill, and that older doctors were rated higher on skill than younger doctors. Whites were rated higher than non-whites across all questions, but there were no other significant associations based on gender, ethnicity or race. Most relevantly for our purposes, the authors found that “the odds of being rated in the top box were highest for obstetricians, second highest for surgeons, and lowest for medicine providers.”
In a Journal of Hospital Medicine article from June 2017, Velez et al. found that HCAHPS scores were not correlated with a broad measure of physician communication skills, the Four Habits Coding Scheme (4HCS), or with any of its four specific “habits:” invest in the beginning, elicit the patient’s perspective, demonstrate empathy, and invest in the end. However, when the authors looked at patients cared for by only a single hospitalist during their stay, the specific habit of demonstrating empathy was, in fact, moderately correlated with the HCAHPS “doctor communication and respect” metric.
Another article published in July 2017 in PLoS One reported that training hospitalists in communication behaviors via a “simulation-based physician communication coaching method focused on specific ‘etiquette-based’ communication behaviors through a deliberate practice framework” was not associated with meaningful improvements in HCAHPS physician communication scores.
Why Might HCAHPS Scores Be Lower for Hospitalist Patients?
There are some structural factors that may contribute to relatively lower patient satisfaction scores for patients attended by hospitalists. Hospitalists are, unfortunately, more or less commoditized: your patient didn’t have any role in choosing you and never met you before the first time you walked into the room. So in addition to being involuntarily stuck in a scary, vulnerable situation, your patient has no basis on which to establish trust in you. Add to this the fact that for many patients, the hospitalist who admitted them isn’t the one who will be caring for them the next day and may not be the one caring for them the day after that. And the typical hospitalist patient has at least one or two consulting physicians in the mix in addition to multiple hospitalists. It isn’t a setup for communication or relationship success.
One of our large health system clients obtained a custom report from Press Ganey in 2015 that compared the difference in top box scores for medical service line patients vs. all inpatients. It showed that the top box score at each percentile was meaningfully lower for medical service line patients – those most likely to be under the care of hospitalists – than for all inpatients:
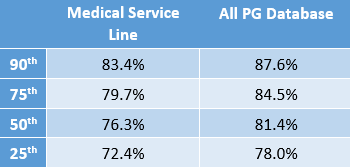
This makes sense to me. Your patients are usually old and frail – and often confused; they come into the hospital with a variety of ill-defined symptoms and a host of chronic co-morbidities. It’s often not clear what their real problem is, and you can’t give a definitive diagnosis or a sure-fire treatment plan. Contrast this with a patient who comes into the hospital for an elective surgical procedure: the treatment team knows exactly what is wrong, what they are going to do about it, what the patient’s course in the hospital will be, and when the patient will be discharged. And that surgical patient always leaves knowing that some remarkable intervention (a “marquee event”) took place that will make their lives better.
How often is there a similar “marquee event” in hospital medicine? Our patients are too often hustled out of the hospital before they feel ready to leave, don’t feel much better upon departure than they did on arrival, and aren’t really sure what exactly the hospitalist did for them while they were here. So it wouldn’t be surprising to me if patients attended by hospitalists tend to have lower hospital-level performance in many or most patient satisfaction domains than patients on other services.
So What Now?
Just because HCAHPS doesn’t really measure individual or group patient satisfaction, and the deck may be stacked against us in terms of the types of patients we care for, this doesn’t mean we should just throw up our hands and walk away. It’s too easy to say, “it’s not our problem.” As vital members of the hospital’s care team, it is our problem – just as much as anyone else’s – to ensure our patients have as good a hospital experience as we can possibly provide for them.
Please don’t let the improper use of HCAHPS survey data impede your commitment to delivering patient-centered, team-based care and communicating effectively with your patients. We all have a responsibility to work diligently with others in the hospital setting to contribute to how our patients feel about their stay in the hospital across all domains. In my next post, I’ll share a couple of innovative strategies hospital medicine groups are using to contribute to improved patient experience by enhancing their communication with patients.



HCAHPS is a poor attempt to characterize physician performance. As a hospitalist, I cannot take HCAHPS seriously as the standards set are more appropriate for a hotel manager or cruise ship director. Also, there is literature showing that higher patient satisfaction = worse outcomes. Want to really make a difference? Don’t embrace this nonsense. Fight back against the inappropriate standards set by CMS.