We have conditioned ourselves to think of readmits in three domains: care transitions (us), patient factors, and community determinants. Guess what? I will give you number four. ER docs. A new study in JHM looked at the role ERs, and ER physicians play in fee for service Medicare readmissions.
The investigators looked at four years of data from Texas hospitals (2008-11), encompassing three million person encounters. They examined patterns of admission after visits to the ED–readmitted on the same day and up to thirty days post initial presentation. They made all the usual adjustments.
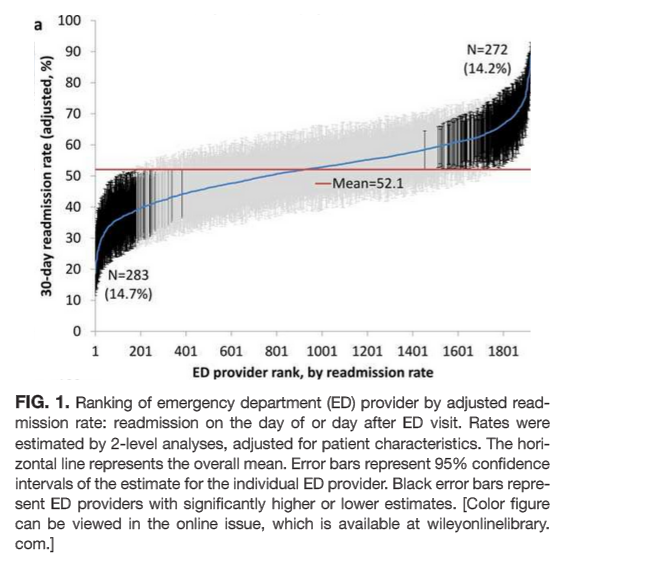
Here’s the ER doc variation money shot:
Fifteen percent of docs on both ends of the readmit spectrum standout. One side gets a cookie, and the other a front row seat in summer school class. The authors sum it up here:
CMS policies hold hospitals accountable for readmissions of the patients they discharge, but do not address the admission process in the ED that leads to readmissions of recently discharged patients. Given the present study, and the fact that the proportion of all hospital admissions that occur through the ED has grown to 44%, consideration of the role of the ED in public policy efforts to discourage unnecessary inpatient care may be appropriate.
In summary, this study shows that a recently discharged patient’s chances of being readmitted depends partly on the ED provider who evaluates them and on the ED facility at which they seek care. ED provider practice patterns and ED facility systems of care may be a target for interventions aimed at decreasing readmission rates.
Another variable to consider when we comprehend the big fix. Culture matters. Individual practice patterns matter. ER docs have different trigger points for bringing folks in and sending them home. I am not surprised and it may be time to add performance measures to their portfolio of “ER transition” quality assessment. Something I am not sure they have undertaken (but I am sure they have considered).



Another important factor in readmits is the effectiveness of patient provider communication. Communication vulnerable patients due to pre-existing medical or developmental conditions, recent onset communication disorders, intervention related communication limitations dealing with respiratory or speech mechanisms, or language different often interfere with patient- provider communication. A recently released book entitled: Patient – Provider Communication: Roles of Speech Language Pathologists and Other Health Providers (Plural Publishing or Amazon) considers communication in a range of medical settings including ICU, acute, rehabilitation, long-term residential and end-of-life. Policies, practices, communication strategies and communication materials are covered in detail.
One problem with your analysis.
Emergency Medicine specialists have NO admission priviliges.
How about the admitting doctors taking responsibility for their bounce backs and physically coming in to evaluate patients. They, then, can discharge these patients well known to them directly from the ED if they deem then not requiring admission.