In April 2017, CMS implemented the new physician specialty code C6, specifically for hospitalists. There has been a lot of confusion about what this means and some uncertainty about why clinicians should bother to use it. Some folks thought initially that it was a new CPT code they could use to bill hospitalist services, which might recognize the increased intensity of services hospitalists often provide to their hospitalized patients compared to many traditional internal medicine and family medicine primary care physicians. Others thought it was a code that was added to the HCFA 1500 billing form somewhere to designate that the service was provided by a hospitalist.
Neither is true. The C6 physician specialty code is one of a large number of such codes used by physicians to designate their primary physician specialty when they enroll with Medicare via the PECOS online enrollment system. It describes the unique type of medicine practiced by the enrolling physician and is used by CMS both for claims processing purposes and for “programmatic” purposes (whatever that means).
It doesn’t change how your claim is processed or how much you get paid. So why bother going through the laborious process of re-credentialing with CMS via PECOS just to change your specialty code? Well, I believe there are several ways in which the C6 specialty code provides value – both to you and to the specialty of hospital medicine.
Reduce Concurrent Care Denials
First, it distinguishes you from a general internal medicine or general family medicine practitioner by recognizing “hospitalist” as a distinct specialty. This can be valuable from a financial perspective because it may reduce the risk that claims for your services might be denied due to “concurrent care” by another provider in the same specialty on the same calendar day. And it’s not just a general internist or family medicine physician that you might run into concurrent care trouble with. I’ve seen situations where doctors completed critical care or cardiology fellowships but never got around to recredentialing with Medicare in their new specialty, so their claims still showed up with an “internal medicine” physician specialty code, resulting in denied “concurrent care” claims for either the hospitalist or the specialist. While Medicare may still see unnecessary overlap between services provided by you and an internal medicine or family physician to the same patient on the same calendar day, you can make a better argument that your services were unique and complementary to (not duplicative of) the services of others if you are credentialed as a hospitalist.
Ensure “Apples to Apples” Comparisons
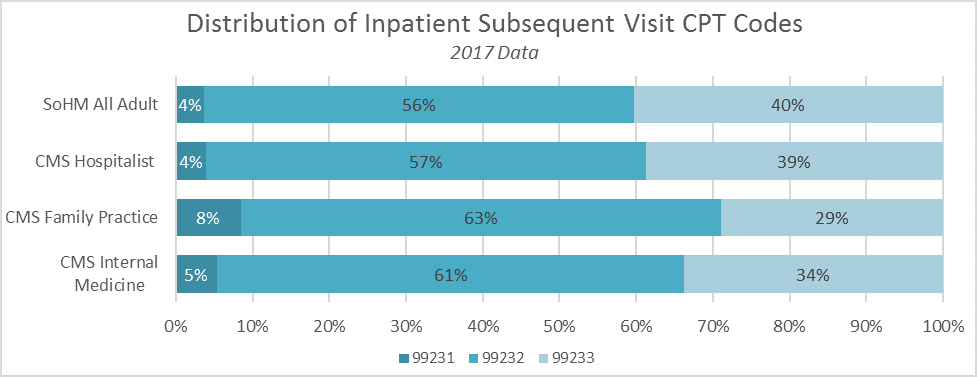
A second reason to re-credential as a hospitalist is to ensure that when CMS looks at the services you are providing and the CPT codes you are selecting, it is comparing you to an appropriate peer group for compliance purposes. The mix of CPT codes reported by hospitalists in the SHM State of Hospital Medicine Survey has historically tilted toward higher-level care than the mix of CPT codes reported by CMS for internal medicine or family medicine physicians. But last year when Medicare released the utilization of evaluation and management services by specialty for calendar year 2017, CPT utilization was shown separately for hospitalists for the first time! The volume of services reported for physicians credentialed as hospitalists was very small relative to the volume of inpatient services provided by internal medicine and family medicine physicians, but the distribution of inpatient admission, subsequent visit, and discharge codes for hospitalists closely mirrored those reported by SHM in its 2018 State of Hospital Medicine Report (see graphic). If you’re going to be targeted in a RAC audit for the high proportion of 99233s you bill, you want to be sure CMS is looking at your performance compared to those who are truly your peers, caring for patients of the same type and complexity as you.
Improve CMS Data Used for Research Purposes
Finally, the ability of academic hospitalists and other health services researchers to utilize Medicare claims data to better understand the care provided by hospitalists and its impact on the overall healthcare system will be significantly enhanced by a more robust presence of physicians who have identified themselves as hospitalists in the PECOS credentialing system. We care for the majority of patients in most hospitals these days, yet “hospitalists” billed only 2,009,869 inpatient subsequent visits (CPT codes 99231, 99232, and 99233) in 2017 compared to 25,903,829 billed by internal medicine physicians and 4,678,111 billed by family medicine physicians. And regardless of what you think about using claims data as a proxy for healthcare services and quality, it’s undeniably the best data set we currently have.
So, let’s work together to build a bigger, better database of hospitalist information at CMS. I urge you to go to your credentialing folks today and find out how you can work with them to get yourself recredentialed in PECOS using the C6 “hospitalist” physician specialty.



Thanks Leslie
Thank you for your effort and sharing this information. Truly worth to read Leslie. Even if you don’t capture all the necessary information, enroll the new physician as soon as possible. According to the Centers for Medicare & Medicaid Services (CMS), incomplete applications will be denied, but the date of the original filing will be preserved.